Articles
- Page Path
- HOME > J Korean Acad Community Health Nurs > Volume 29(1); 2018 > Article
- Original Article Regional Factors on the Self-rated Health of Wage Workers
- Minjung Kwon1, Eunsuk Choi2
-
Journal of Korean Academy of Community Health Nursing 2018;29(1):21-32.
DOI: https://doi.org/10.12799/jkachn.2018.29.1.21
Published online: March 31, 2018
1College of Nursing, Kyungpook National University, Daegu, Korea
2College of Nursing · Research Institute of Nursing Science, Kyungpook National University, Daegu, Korea
-
*Corresponding email:
eschoi2007@knu.ac.kr
- 525 Views
- 7 Download
- 0 Crossref
- 0 Scopus
Abstract
PURPOSE
This study attempted to identify regional disparities of self-rated health among Korean wage workers and to investigate the influencing factors on them.
METHODS
The study subjects were 25,069 workers in 16 regions who were extracted from the 2014 Korean Working Condition Survey (KWCS). A multilevel analysis was conducted by building hierarchical data at individual and regional level.
RESULTS
In this study, ‘financial autonomy rate’ and ‘current smoking rate’ were identified as regional factors influencing the workers' self-rated health. When the socio-demographic and occupational factors of the workers were controlled, ‘current smoking rate’, a health policy factor, explained the regional disparity of workers' health status.
CONCLUSION
We found that the health status of workers can be affected by the health behavior level of the whole population in their residential area. In order to improve the health status of working population and to alleviate their regional health inequalities, it is necessary to strengthen macro and structural level interventions.
| J Korean Acad Community Health Nurs. 2018 Mar;29(1):21-32. English. Published online Mar 30, 2018. https://doi.org/10.12799/jkachn.2018.29.1.21 | |
| © 2018 Korean Academy of Community Health Nursing | |
| Minjung Kwon,1 and Eunsuk Choi2 | |
|
1College of Nursing, Kyungpook National University, Daegu, Korea. | |
|
2College of Nursing · Research Institute of Nursing Science, Kyungpook National University, Daegu, Korea. | |
Corresponding author: Choi, Eunsuk. College of Nursing, Kyungpook National University, 680 Gukchaebosang-ro, Jung-gu, Daegu 41944, Korea. Tel: +82-53-420-4936, Fax: +82-53-421-2758, | |
| Received August 06, 2017; Revised January 18, 2018; Accepted January 26, 2018. | |
|
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by- | |
|
Abstract
| |
|
Purpose
This study attempted to identify regional disparities of self-rated health among Korean wage workers and to investigate the influencing factors on them.
Methods
The study subjects were 25,069 workers in 16 regions who were extracted from the 2014 Korean Working Condition Survey (KWCS). A multilevel analysis was conducted by building hierarchical data at individual and regional level.
Results
In this study, ‘financial autonomy rate’ and ‘current smoking rate’ were identified as regional factors influencing the workers' self-rated health. When the socio-demographic and occupational factors of the workers were controlled, ‘current smoking rate’, a health policy factor, explained the regional disparity of workers' health status.
Conclusion
We found that the health status of workers can be affected by the health behavior level of the whole population in their residential area. In order to improve the health status of working population and to alleviate their regional health inequalities, it is necessary to strengthen macro and structural level interventions. |
|
Keywords:
Multilevel analysis; Occupational health; Health status disparities; Residence characteristics; Health behavior
|
|
|
INTRODUCTION
|
1. Background
Workers play an important role in organizational productivity and social development. Therefore, as part of the efforts to maintain and promote the health of workers, many researchers have attempted various approaches to identify the influencing factors that explain their health and to develop interventions for them.
Among the various perspective of health, Rose has proposed a population-based approach, which suggests that individuals belong to the society and population and the explanation of the population's health should include the social context [1]. Individuals' health is dependent not only on personal risk factors but also on the environmental characteristics of the area surrounding them. For example, the social environment influences individuals by forming norms, reinforcing specific types of social control, and providing or limiting environmental opportunities for individuals to participate in certain behaviors [2]. Likewise, workers' health can be explained by the contextual factors of the population they belong to as well as the micro-level individual and workplace characteristics. Many studies on work and health have mainly dealt with occupational epidemiology focused on individual risk factors and occupational characteristics (physical and chemical risk factors) of workers, and more recently, attention has been paid to various factors including ergonomic and psychosocial work environments [3, 4].
The region is an important analytical unit where various factors work together and thereby form the quality of life of the local residents. As the interest in the place has been increased since 1990, some studies have pointed out that existing studies focused only on individual units and claimed that the region itself needs to be considered [5]. For example, the socio-economic environment of a residential area have been observed to be significantly associated with health behaviors and health status levels [6], and this association may be independent of the individuals' socio-economic characteristics [7]. These contextual effects at the regional level are independent effects of the higher analytical unit factors explaining the individuals' health behaviors and health status levels after controlling for the characteristics of members inherent in the higher analytical unit called the community, and are distinguished from the compositional effect exhibited by the group of individuals having specific characteristics.
The importance of the context for health interventions in the nursing area has long been recognized and has become evident due to an increase in community-based interventions. However, to date, the social health distribution and the impact of regional factors in relation to the health of workers have not been sufficiently taken into account in the studies of workers and interventions for them in the field of nursing. Recently, multidimensional analysis of the health-related factors of workers based on ecological models has been conducted in some studies, but they have been mainly focused on clarifying individuallevel and organizational-level factors [8, 9].
On the other hand, in other fields, studies have been accumulated to elucidate social determinants of health with a growing ecological interest in the social distribution of health. In previous studies that attempted multi-level approaches, various types of factors such as social class including socioeconomic status (SES)[10], social capital, or social relationships [11, 12] have been discussed as the social determinants of health. Various factors that represent the social structure, intervention level, and health outcomes are known to affect the differences in the health status of the population [13], and related studies have reported that regional variations in mortality, regional-level education, the financial autonomy rate, the current smoking rate, and the walking exercise rate are related to them [14]. However, regional variables that consistently affect individuals' health have not been systematically structured yet, and no studies which tested the regional variables for working population have been reported yet.
On the other hand, Benach et al.[15], explained that employment status, working conditions, and economic and policy factors of society may influence the health inequalities of workers through complex mechanisms, using theoretical models of employment relations and health inequalities (micro & macro level). The theory suggested by Benach et al.[15] has presented micro-level and macro-level contextual factors related to the health outcomes of workers. Based on these theoretical factors as well as Rose's population-based approach [1], this study intended to verify the regional factors explaining regional differences in the health status of workers. Therefore, we attempted to elucidate regional variables as the determinants of health status of workers, adjusting the indiviindividual-level factors such as socio-economic characteristics, working conditions, and occupational risk factors. The research question to be explored in this study is ‘What are the regional factors that affect the health status of workers?’
In this study, multilevel analysis was conducted as the methodology taking into account multidimensional effects including individual, environmental, and policy factors. Multilevel analysis makes it possible to simultaneously evaluate the associations between the determinants measured at various levels and health when factors affecting individuals' behaviors are present not only at the individual level but also at a higher level, such as a group or region, and may be suitably used as a research model for explaining the regional differences in the health status of workers. The data of the Korean Working Condition Survey used in this study are the sample data of Korean workers, and they allow for verification of various factors related to the employment conditions of workers. Therefore, this study aimed to present the grounds and direction of the regional-level approach to the interventions for workers through the multi-level analysis using the data of the Korean Working Conditions Survey and the regional factor indicators of the Statistics Korea.
2. Purpose
This study was conducted to determine whether the regional factors related to the areas where workers reside affect the health status of workers independently of the individual characteristics. The hypotheses of this study are as follows:
The self-rated health of workers will vary according to regional factors.
Regional factors will have a significant impact on workers' self-rated health.
When controlling for individual factors, regional factors will have a significant impact on workers' self-rated health.
|
METHODS
|
1. Study Design
This study is a descriptive study to elucidate individual and regional factors that affect the self-rated health of workers, and multi-level analysis was performed using hierarchical data based on the theoretical model of Benach et al. [15], which explains workers' health inequalities (Figure 1).
|
2. Subjects and Data Collection
In this study, two-level data were collected for the construction of hierarchical data set. For the level 1 research data, the data from the 4th Korean Working Condition Survey (2014) conducted by the Korea Occupational Safety and Health Research Institute (KOSEF) was utilized. The Korean Working Condition Survey has been carried out since 2006 with the approval of the Statistics Korea (approval No. 38002), and it is a large-scale survey that provides the overall information on the work environment, including employment type, working conditions, type of occupation, and exposure to occupational risk factors, benchmarking the European Working Condition Survey. In this study, we used coded raw data excluding the data for which it is possible to estimate the subjects provided after the review by the data provider organization. The population was employed people aged 15 years or older in all households in Korea. The survey population was sampled through the secondary probability proportion stratified cluster sampling method by reflecting the criteria of the 2010 Population and Housing Census. In this study, among a total of 50,007 persons of the raw data, only wage workers aged 20 years or older were included. Among them, 25,069 workers were included in the final analysis excluding the residents in Sejong City, for whom it was difficult to produce regional indicators, soldiers, and missing data for major variables.
The level 2 regional units were classified based on the area codes classified in the Korean Working Condition Survey, and the regional units of 16 cities and provinces excluding Sejong City were included in the analysis. The data of each region were based on the statistical data by region of the Statistics Korea and the results of the research reports of the Korea Institute for Health and Social Affairs.
3. Measures
1) Dependent variable: self-rated health
The dependent variable is the self-rated health of workers, and it was measured on a 5-point scale by rating it as ‘very good’ to ‘very bad’ in response to the question ‘How is your health in general?’ Self-rated health is a health indicator that assesses the perception of overall health status, and the association between self-rated health and objective assessment of individuals' physical health and functional status has been confirmed [16]. In this study, if the subjects rated their health status as ‘fair’ to ‘very good’, they were classified as the ‘fair group,’ and if they assessed their health status as ‘bad’ to ‘very bad’, they were classified as the ‘poor group.’ In this way, the data were analyzed as binary data [17].
2) Individual-level factors
In this study, individual-level demographic factors included gender, age, and education level. As for gender, male and female were converted into dummy variables. As for age, the subjects were divided into the age groups of 20~34 years, 35~54 years, and 55 years or older in the univariate analysis, but a continuous variable was applied in the multilevel model. The education level was classified into middle school graduation or lower, high school graduation, and junior college graduation or higher.
Occupational factors included average monthly income, employment type, weekly working hours, atypical work, exposure to occupational risk factors, social support, and workplace size. The average monthly income was divided into less than 1 million won, 1~1.99 million won, 2~2.99 million won, and 3 million won or more. The employment type was classified into regular and non-regular workers. The weekly working hours were divided into less than 35 hours, 35~47 hours, and 48 hours or more. The presence of atypical work was measured according to whether the subject works shifts, works overtime in the evening, or works on Saturday or Sunday at least once a month. As for the exposure to occupational risk factors, regarding the question about physical risk factors (vibration, noise, high temperatures, or low temperatures), chemical risk factors (dust, steam, or chemicals), ergonomic risk factors (tiring or painful postures, dragging, pushing or moving heavy objects, or repetitive hand or arm movements), and psychological risk factors (dealing directly with non-co-workers including customers or dealing with angry customers or patients), for each category of risk factors, the responses were classified into ‘yes’ and ‘no’ according to whether the subject is exposed to at least one kind of risk factor during more than half of work hours. With respect to the level of social support from colleagues and supervisor, regarding the item ‘My colleagues/supervisor help(s) and support(s) me,’ the responses ‘Always agree’ to ‘Sometimes agree’ were classified as ‘high’ and other responses were classified as ‘low.’ For the size of the workplace workers belong to, it was divided into less than 50 persons and 50 persons or more.
3) Regional-level factors
For the regional-level variables, the ‘number of physicians working in medical institutions per 1,000 people’ among e-Regional Indicators 2013 provided by the Statistics Korea [18] and some of the Korean Health Inequalities Indicators presented by the Korea Institute for Health and Social Affairs in 2014 were used by converting the data into those for 16 cities and provinces. The Korean Health Inequalities Indicators [13] were selected by dividing them into social structural factors, intervention factors, and health outcome factors through experts' review of health determinants according to the mechanisms underlying health inequalities. In this study, among these indicators, regional-level factors were selected according to the theoretical constitution of this study with a focus on the factors related to regional deprivation, social integration and social capital, living environment, health lifestyle, and health care services, as presented below.
The social and health policy factors included the ‘current smoking rate’ and ‘high-risk drinking rate’ of 16 cities and provinces. These were presented as social intervention factors among The Korean Health Inequalities Indicators [13], and generally used as the indicators of public health policies.
Socioeconomic factors at the regional level included the ‘financial autonomy rate’ and ‘harmful environment work rate’. The ‘financial autonomy rate (FAR)’ represents the social structural characteristics of the region and is used as an indicator of regional deprivation [13]. The ‘financial autonomy rate (FAR)’ is more generally used than the financial independence rate (FIR) as an indicator of the soundness of the finance of local governments, and it shows how much of the total revenue the local governments can use autonomously at their own discretion. In this study, the data of each of seven regions were used by assigning them to 16 cities and provinces.
As the health system factor, the ‘number of physicians working in medical institutions per 1,000 people’ of 16 cities and provinces was used as a indicator of the quantitative level and accessibility of healthcare service resources [18].
The regional social network factor was analyzed using ‘social trust’ as an indicator of social capital and social integration [13].
4. Data Analysis
In this study, χ2 test and t-test were conducted through PASW statistics 24.0 (IBM Co., Armonk, NY, USA) to examine the difference in self-rated health according to individual-level and group-level factors of workers, and correlations between regional-level variables were determined by Pearson's correlation coefficient.
For the hierarchical analysis of individual- and regional-level variables, HLM 7.01 for Windows (SSI Inc., Skokie, IL, USA) was used, and multi-level logistic analysis was performed assuming the Bernoulli distribution of dependent variable. In the multi-level model, only variables of which statistical significance was confirmed through univariate analysis were entered (p<.05). For age, which is an individual-level variable, and regional-level variables, grand-mean centering was performed, which makes it possible to maintain the regional variations of variables and estimate the effects of regional-level variables more efficiently. In Model 1, which is the null model that does not include explanatory variables, the significance of regional differences for the dependent variable was determined and the validity of model setting was verified by calculating regional variance. In Model 2 (means outcome model) and Model 3 (random effect ANCOVA), regional-level and individual-level variables were applied, respectively, to examine the decrease in the regional-level variance. In Model 4, which is the variance component model including both individual-level and regional-level variables, the regional variables that explain the self-rated health of workers were identified while controlling for individual-level factors. The multi-level model was estimated by the Penalized quasi-likelihood (PQL) method. The distribution of major variables is shown in Table 1.
|
|
RESULTS
|
1. General Characteristics of Subjects
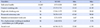
In terms of self-rated health, a total of 25,069 subjects were divided into the fair health status group of 24,020 persons (96.5%) and the poor health status group of 866 persons (3.5%). The average age of the subjects was 43.78±12.67 years, and males accounted for 51.5%. As for the level of education, 50.7% of the subjects were junior college graduates or higher. With respect to occupational characteristics, the proportion of workers earning the average monthly income of 1~1.99 million won was the highest (36.4%), and regular workers accounted for 77.0%. 52.7% of the subjects worked 35~47 hours per week, and 61.1% had atypical work experience. Regarding the exposure to occupational risk factors, the experience rate of the ergonomic risk factor was the highest at 59.5%. 11.2% and 14.8% of the respondents had low social support from their colleagues and supervisor, respectively. Regarding the workplace size, 72.7% were working in the workplaces with 50 employees or more (Table 2).
|
2. Individual- and Regional-level Factors and Workers' Self-rated Health
There were significant differences in the self-rated health of workers between the two groups according to demographic factors such as gender, age, and education level among the individual-level factors (p<.001). In terms of occupational characteristics, it was found that the group with the average monthly income of 3 million won or more and the group working for 35~47 hours per week were most likely to belong to the group with good self-rated health, and there was a significant difference in the self-rated health status between the two groups according to the employment type and the level of social support (p<.001). As for the relationship between self-rated health and exposure to occupational risk factors, there were differences in self-rated health according to the exposure to each of physical, chemical, and ergonomic risk factors (p<.001), but there was no statistical difference according to the exposure to the psychological risk factor (p=.139). In addition, there was no significant difference in the self-rated health of workers depending on the size of the workplace (Table 2).
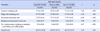
The self-rated health of workers according to regional-level factors was obtained through a single dimension analysis by assigning regional-level variables according to the area codes assigned to individuals (Table 3). There were significant differences in the self-rated health of workers according to the current smoking rate, financial autonomy rate, number of physicians working in medical institutions per 1,000 people, and social trust. The harmful environment work rate and high-risk drinking rate in the region were not significantly related to the difference in self-rated health of workers.
|
3. Effects of Individual- and Regional-level Factors on Workers' Self-rated Health
Based on the results of the univariate analysis of the individual- and regional-level variables, variables other than atypical work, the exposure to psychological risk factors, and the size of the workplace among individual-level variables and harmful environment work rate, and high-risk drinking rate among regional level variables were entered in the multi-level model. As a result of correlation analysis of the regional-level variables, there was no significant correlation between the variables (r<0.5, p<.05), and multicollinearity was not detected, so the results about this are not presented separately in this study.
Model 1 is the unconditional model where individual- and regional-level variables were not entered, and there were statistically significant regional differences in the self-rated health of workers (χ2=111.68, p<.001)(Table 4). The level 2 variance (τ) was 0.1141 and the ICC value of the basic model was 0.0335 as a result of calculating the value by applying the theoretical residual (π2/3) for the level 1 of the logistic model. Although the general suggested criterion for the ICC value is 0.05 or higher, multilevel analysis can be carried out if there are empirical study results on regional variations [19]. Considering the relatively small sample size at the regional level in the data of this study, the influences of variables were confirmed by verifying the variables in a stepwise manner based on the statistical significance of the variance value (τ).
|
In Model 2 in which only the regional level variables were applied, the financial autonomy rate (OR=1.03, p<.05) and current smoking rate (OR=0.97, p<.05) significantly explained regional differences in the self-rated health status of workers. In other words, the probability that the self-rated health of individual workers was good increased by 1.03 times when the financial autonomy rate of the region was increased by one unit, and decreased by 0.97 times as the current smoking rate of the region became lower. The ICC value for Model 2 was 0.0079, and the regional level variables explained 77% of the level 2 variance (τ) in the initial model, when individual factors were not taken into account (χ2=36.58, p<.001).
In Model 3, in which only the effects of individual-level variables were verified (χ2=84.64, p<.001), the odds ratio decreased by 0.75 times for women, by 0.96 times as age was increased by one year, by 0.77 times in case of weekly working hours of 48 hours or more, and by 0.80 and 0.51 times, respectively, when exposed to chemical and ergonomic occupational risk factors, showing that they are factors influencing workers' self-rated health negatively. On the contrary, the odds ratio was 1.97 times higher when the education level was junior college graduation or higher. Also, it increased with an increase in the average monthly income, and especially, it was 1.93 times higher in the case of the average monthly income of 2~2.99 million won. In addition, when the levels of social support of colleagues and supervisors were high, the odds ratio was 1.32 times and 1.26 times higher, respectively, indicating a higher likelihood that the self-rated health status of workers is good. These individual-level variables accounted for 18.4% of the regional variance (τ).
In Model 4, both individual- and regional-level variables were entered, and it was found that there were regional differences in the health status of workers with adjusted individual factors. The level 2 variance (τ) was lowered to 0.0316, and the input variables explained 72.3% of the total regional variance and were statistically significant (χ2=39.29, p<.001). The significance of the variables was not different from the results in Model 3, but overall, the odds ratio decreased slightly. In the case of regional-level variables, only the current smoking rate had a statistically significant effect on the self-rated health of workers (OR=0.97, p<.01), and the financial autonomy rate was not significant after entering individual-level variables (Table 4).
|
DISCUSSION
|
Based on the theoretical model of Benach et al. [15], which explained the health inequality of workers, this study attempted to examine the regional differences in the self-rated health of workers and clarify the regional variables explaining them. In the multi-level model confirmed through the construction of hierarchical data, for the regional-level variance (τ) at the last stage, there was the decrease of 72.3% of the initial model and 66.1% of Model 3, where only the individual-level variables were applied. With reference to Model 2, where only regional variables were confirmed, the ‘financial autonomy rate’ of the region did not have a statistically significant effect after controlling for individual-level variables including socioeconomic factors, but the ‘current smoking rate’, which is an indicator of interventions at the regional level, was found to be still significant.
Smoking is known to be a major risk factor for non-infectious diseases such as cardiovascular disease, diabetes, cancer and chronic respiratory disease. According to the data of 2015, the daily smoking rate of males aged 15 years or older is reported to be 31.4%, which is higher than the OECD average of 23.9%[20]. In studies of workers, smoking has been identified as a factor that lowers the perceived self-rated health status (OR: 1.5~1.56) [21, 22]. However, in previous studies which confirmed the contextual effects of various health outcomes including self-rated health, sufficient investigation into the impact of the level of health behaviors of the group on the health status of individuals, particularly, on the health status of workers, has not been conducted. The results of this study, which were obtained with individual risk factors of workers adjusted, indicate that the level of health behaviors of the entire region may be an influencing factor explaining the health status of individuals.
Smoking is not only an individual risk factor, but it also creates external effects such as secondhand smoking and indoor air pollution, so it can generate a protective effect on the health of the population by lowering the overall prevalence through interventions, just like vaccination. However, to date, health interventions have been intensively conducted for a relatively small number of people such as schools, workplaces, or high risk groups, and the overall population in the region has not been sufficiently considered.
Individual-level interventions target the boundary levels of the health behavior distribution extremes, but structural-level interventions for neighborhoods, workplaces, and communities can shift the mean value of the distribution [23]. Among the various mechanisms that affect workers' health inequalities, health behaviors at the regional level can be determined through public policies, which lead to other public health outcomes, and have an impact on the life experiences of different social groups [15]. In this regard, Cohen et al. [23] suggested that the four factors that constitute a structural model of population-level health behavior are availability, physical structures, social structures and policies, and media and cultural messages. Specifically, in relation to current smoking policies, they include intervention efforts, such as adjustment of cigarette prices, insertion of warning messages, designation and promotion of no smoking areas voluntarily or by regulations, and creation of norms of health behaviors.
In this context, analysis of the influence of smoking at the regional level as an intervention factor indicates the necessity to expand the range of nursing intervention and to apply a complex approach to the community. Therefore, the results of this study suggest that in order to improve the health of workers and alleviate the level of their regional health inequalities, it is necessary to further strengthen intervention efforts at the macro-structural level as well as at the individual level. In addition, in relation to the interventions for regional factors, including smoking, it is necessary to establish a strategy to fundamentally enhance the accessibility and feasibility of interventions within the context of social policies, through efforts such as linking community health promotion programs with workplaces, rather than nursing being in charge of a part of the existing education, counseling, or treatment-based approach.
On the other hand, in the previous studies of self-rated health using multi-level models, ‘social capital’, which is composed of the characteristics of social organizations such as community cohesion and networks, was emphasized rather than the health behavior level or intervention-related factors of the region. Social capital may affect individuals' health through spreading health-related information and behavior patterns or affecting access to services and facilities, or through psychosocial processes such as affective support, and it was found to be a mediator in the relationship between socioeconomic factors and health [11, 12, 24].
In a previous study of Kim [25], which investigated the self-rated health of community residents, regional-level ‘social trust’ was found to be a determinant of vulnerable health status, but the ‘financial independence rate’, ‘number of health care resources’, ‘poverty rate’, and ‘organizational network’ were found to have no significant influence. In this study of workers, the variables representing the health system factor and social network factor were tested in addition to the ‘financial autonomy rate’ and ‘current smoking rate’. The ‘number of physicians working in medical institutions per 1,000 people’ and ‘social trust’ were found to show statistical differences in the univariate analysis, but they did not have a significant impact in the multi-level model. In addition, a study of the influence of other ecological factors on local residents investigated the impacts of regional social infrastructure and the neighborhood living environment, and the accessibility to convenience facilities such as parks was also found to explain self-rated health [26]. Since there have been very few studies on workers and regions so far, there are not sufficient previous study results for comparative analysis. Moreover, since the regional factors investigated in this study were also limited, it is necessary to investigate the effects of other potential intervention factors in future studies.
Next, at level 1, gender, age, education level, average monthly income, weekly working hours, exposure to occupational risk factors, and support from colleagues and supervisor were found to be the determinants of workers' self-rated health. The association between such individual-level factors and self-rated health of workers has also been confirmed by recent studies of self-rated health based on large-scale data on workers such as the Korean Working Conditions Survey and the Korean Labor and Income Panel Study [10, 27].
Socioeconomic status has been reported to be a major determinant of health inequalties [28]. In this study, the group with the monthly average income of 2~2.99 million won and the group with the education level of junior college graduation or higher were most likely to assess their subjective health status as good. In the final model, when the individual-level variables were included, the explanatory power of the regional-level variable was lost, so this is judged to be the compositional effect of the population, not the regional contextual effect of the socioeconomic dimension for the health status of workers. In this regard, in the multi-level studies of community residents, it has been reported that although socioeconomic factors explained self-rated health at both individual and regional levels, individual and household economic factors had greater effects than regional factors such as material deprivation and income inequality [17, 22]. Taken together, the findings of this study and previous studies described above suggest that socioeconomic status of individual workers has a more important effect on health outcomes than the overall effect of the region on the socioeconomic dimension.
The work environment and lifestyle factors of workers were found to account for two-thirds of the social gradient in self-rated health in a Danish cohort study, and among the factors, the work environment factor was found to be the largest contributing factor [29]. In this study, the exposure to occupational risk factors was identified as a factor that significantly lowered the self-rated health of workers, which is consistent with the results of previous studies [27, 28]. On the other hand, the univariate analysis did not show differences in the self-rated health of workers depending on the ‘harmful environmental work rate’ at the regional level, and it is considered necessary to perform verification for relevant factors at both the regional and individual levels to clearly explain such contrast. For example, individuals who are engaged in health risk behaviors such as smoking tend to be simultaneously exposed to the harmful work environment, and such health risk behaviors have been reported to be high in the working class or low-income workers [29, 30]. However, in this study, individual-level lifestyle factors of workers and the interaction between regional-level variables were not considered. The health behaviors of individuals and the group may affect workers' health outcomes through different pathways, and future research efforts should be directed at explaining the comprehensive mechanism taking into account these multi-level influences. Collectively, these individual-level variables accounted for 18.4% of the total regional variance of the initial model.
In this study, it was confirmed that the ‘current smoking rate’ at the regional level had an effect as a social intervention factor when individual-level socio-demographic and occupational factors explaining the self-rated health of workers were considered comprehensively. The community as the target for nursing care may refer to a specific area, group, or organization, or it may be a mixture of all three. The prevention and management of chronic diseases are becoming increasingly important in modern society, and widespread regional-level interventions can be more effective than individual-level interventions that need to be intensively conducted and require high costs. In this regard, the results of this study are thought to show the validity of regional health interventions beyond the interventions for individuals or workplaces.
A significant result of this study is that it confirmed regional disparities in the health status of workers and elucidated the regional factors that have not received attention in the health intervention for workers. However, one of the limitations of this study is that we could not test various factors related to workers' health since this study was conducted using secondary data, so further studies are required to systematically investigate the variables that can clearly reveal the regional effects and confirm their interactions. In addition, the regional-level analytical units of this study were 16 cities and provinces, and the regional-level variance which can show differences in the health status was not large enough. Future studies need to secure a sample size that can more clearly demonstrate regional differences and effects of interventions, taking into account the scope of the region sharing social elements for health and having group homogeneity. It is also necessary to examine whether the region surveyed was the residence area that represented the actual living sphere of workers. Finally, the self-rated health used as the dependent variable in this study is one of the most general indicators to assess the health status of a population, but there is a need to verify it through the indicators that can be used in evaluation, considering the application of health interventions in the future. Therefore, extended tests through the objective variables that better represent the health of workers are needed.
|
CONCLUSION
|
Health interventions for regions are provided within the context of the overall health management system, and the unique role of nursing care in the community has not been clearly defined or confirmed compared to other areas. In addition, little attention has been paid to the region as the target for interventions despite its widespread impacts.
In this study, the regional differences in the self-rated health of wage workers were verified from a population-based perspective, and it was found that the level of health behavior of the entire region can be an influencing factor explaining their health status whether individual risk factors were considered or not. The health behaviors and health status of individual workers may be affected by the interaction of the family, community, and health management system and cultural norms. The discussions about the impact of smoking as an intervention factor at the regional level shown the necessity for applying a multidimensional approach to the community and shifting and broadening the perspectives about this.
Comprehensive health interventions at the regional level may have a protective effect on the health of the population, including workers, and may be a more appropriate approach to the current trend of the increase in the overall risk of chronic diseases. The multi-level approach attempted in this study suggests the possibility of the attempt to test new variables in community-level research. In the future, further studies are required to explore the various variables that make it possible to establish specific interventions considering social, environmental and policy factors.
|
References
|

 KACHN
KACHN





 PubReader
PubReader Cite
Cite