Articles
- Page Path
- HOME > J Korean Acad Community Health Nurs > Volume 31(4); 2020 > Article
- Original Article The Effect of Unemployment in Depression by Age Group: Using 12 States' Data from the Behavioral Risk Factor Surveillance System
- Kyung Mi Woo, Zhi Sun Zhang
-
DOI: https://doi.org/10.12799/jkachn.2020.31.4.436
Published online: December 31, 2020

2Master in Public Health, Mailman School of Public Health, Columbia University, New York, USA

- 558 Views
- 20 Download
- 2 Crossref
- 0 Scopus
Abstract
Purpose
This study aims to explore the association between unemployment and depression in people from different age groups ranging from 18 to 65 years old.
Methods
This study used a cross-sectional design. We performed bivariate analysis and multivariable logistic regression on the 2010 Behavioral Risk Factor Surveillance System (BRFSS) data from 12 states in the United States.
Results
On a sample comprised of n=53,406 individuals, of whom 2,546 (7.8%) were identified as being depressed and 3,448 (10.6%) as unemployed, we found that individuals aged 61~65 years have a lower depression risk compared to those aged 18-25 after adjusting for other variables including employment status. However, people from 61~65 have higher increased risk of depression when unemployed compared to other age groups in all three models tested (3.95 times higher in unemployed people in model 1, and 2.81 times higher in model 2 and model 3).
Conclusion
Our findings indicate that there may need to be more focus on older adults who are unemployed, with associated support services for their mental health. The results of our study indicate that although older adults are less likely to be unemployed, there are more likely to experience depression if they are unemployed (once other confounding factors are taken into account) than younger adults. Policies and interventions can be developed to address not only the physical difficulties but also the mental challenges with which older adults can be at risk facing in case of unemployment.
| J Korean Acad Community Health Nurs. 2020 Dec;31(4):436-446. English. Published online Dec 28, 2020. https://doi.org/10.12799/jkachn.2020.31.4.436 | |
| © 2020 Korean Academy of Community Health Nursing | |
| Kyungmi Woo,1 and Zhisun Zhang2 | |
|
1Assistant Professor, College of Nursing · The Research Institute of Nursing Science, Seoul National University, Seoul, Korea. | |
|
2Master in Public Health, Mailman School of Public Health, Columbia University, New York, USA. | |
Corresponding author: Woo, Kyungmi. College of Nursing, Seoul National University, 103 Daehak-ro, Jongno-gu, Seoul 03080, Korea. Tel: +82-2-740-8828, Fax: +82-2-740-8828, | |
| Received August 02, 2019; Revised July 24, 2020; Accepted October 20, 2020. | |
|
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by- | |
|
Abstract
| |
|
Purpose
This study aims to explore the association between unemployment and depression in people from different age groups ranging from 18 to 65 years old.
Methods
This study used a cross-sectional design. We performed bivariate analysis and multivariable logistic regression on the 2010 Behavioral Risk Factor Surveillance System (BRFSS) data from 12 states in the United States.
Results
On a sample comprised of n=53,406 individuals, of whom 2,546 (7.8%) were identified as being depressed and 3,448 (10.6%) as unemployed, we found that individuals aged 61~65 years have a lower depression risk compared to those aged 18-25 after adjusting for other variables including employment status. However, people from 61~65 have higher increased risk of depression when unemployed compared to other age groups in all three models tested (3.95 times higher in unemployed people in model 1, and 2.81 times higher in model 2 and model 3).
Conclusion
Our findings indicate that there may need to be more focus on older adults who are unemployed, with associated support services for their mental health. The results of our study indicate that although older adults are less likely to be unemployed, there are more likely to experience depression if they are unemployed (once other confounding factors are taken into account) than younger adults. Policies and interventions can be developed to address not only the physical difficulties but also the mental challenges with which older adults can be at risk facing in case of unemployment. |
|
Keywords:
Depression; Unemployment; Aged; Age groups; Behavioral risk factor surveillance system
|
|
|
INTRODUCTION
|
Depression can happen at any age, but often begins in adulthood [1] and can reduce life quality and increase the risk of health problems [2]. Work is essential in daily life and having satisfying work is key for favorable health [3]. Many studies have shown that employment protects psychological health by providing meaning to people's lives [4].
In regards to the relationship between unemployment and depression, several research papers show that unemployment is associated with an increased risk of depression [2, 5, 6, 7, 8]. A recent study by McGee and Thompson [2] using national 2010 Behavioral Risk Factor Surveillance System (BRFSS) data reported that the odds of depression were about 3 times higher for unemployed than employed emerging adults (18~25 years).
Although there are some studies that have suggested age could be a potential risk factor for depression, there appears to be a lack of research exploring potential relationships between employment status and depression across different age groups in adulthood. A study tested the roles of duration and age on the relationship between unemployment and psychological ill-health [9]. The relationship among 954 unemployed adults in 5-year spans from 16 to 64 was explored, and the results showed that the association between length of unemployment and psychological ill-health was the strongest in the middle-age groups, while the association was lower for the youngest and oldest groups [9]. A cross-sectional survey found that older age was a risk factor (OR 1.43) associated with increased depression in the short-term unemployed and was a significant risk factor (OR 2.51) for those unemployed long-term [10].
Given these mixed and inconclusive findings, the aim of this study was to explore the association between unemployment and depression among people in different age groups ranging from 18 to 65 years old.
|
METHODS
|
We used 2010 Behavioral Risk Factor Surveillance System (BRFSS) data from the United States (US) to conduct this secondary data analysis. The BRFSS is a national survey conducted every year to assess health risk behaviors among the non-institutionalized US adult population (age 18 years and older). The BRFSS includes data from all 50 states as well as the District of Columbia, Puerto Rico, and the US Virgin Islands. However, depression data is not included in the routine set of survey questions and has to be selected by each state as an optional module. Therefore, only data from 12 states (Arizona, Georgia, Hawaii, Indiana, Louisiana, Mississippi, Missouri, Nevada, South Carolina, Vermont, Wisconsin, and Wyoming) that collected depression prevalence data in 2010 were included in this study. This study is a secondary data analysis of public access data which does not require Institutional Review Board (IRB) approval.
1. Population
For age group classification, we used preferred terms for age groups from Academic Search Premier & Soc-Index, which provides life stage groups. As per the index, people 18~25 years of age are classified as young adults, 25~40 years of age as adulthood, 40~60 as middle age, and 60+ as older people. We assumed that unemployment would not be relevant to individuals who are retired; we therefore considered people ages 65+ as retired and excluded them from our analysis. Of the total population from eligible states (N=79,629), we extracted data on individuals aged 18~65 years (inclusive) for our sample (N=53, 406) and categorized them into the four age groups as defined above (Figure 1).
|
2. Measures
The dependent variable was depression. We drew upon the data from the optional module, which uses eight variables to measure depression, to create a depression score based on the Patient Health Questionnaire (PHQ-8) [11, 12]. The questions ask about depressive symptoms over the previous 2 weeks. For example, “Over the last 2 weeks, how many days have you had little interest or pleasure in doing things?” For each question, individuals received a score between 0 and 3 depending on the number of days they reported having the specific depressive symptom. Those who responded that they had had a depressive symptom for 0 days or 1 day received a score of 0. Those who responded that they had had a depressive symptom for 2 to 6, 7 to 11, or 12 to 14 days, inclusive, received scores of 1, 2, or 3, respectively. The scores for each question were summed. To construct a binary dependent variable, subjects were classified as depressed if the depression score was greater than or equal to 10[12].
The main independent variable of interest was employment status. Those individuals who responded to the survey that they had been out of work for either less than 1 year or more than 1 year were classified as unemployed. Respondents who indicated they were “employed for wages” or “self-employed” were classified as employed.
Potential confounding variables were included in the multivariable logistic model because of their association with both depression and employment status. These were disability status, smoking status, health insurance status, body mass index (BMI), and sociodemographic status (sex, race/ethnicity, marital status, education, and income level). Most of the potential confounding variables were selected based on previous work by Brown and colleages [13] and McGee and Thompson [2], which examined relationships between unemployment and mental health among adults.
For the disability status variable, we used two variables (QLACTLM and USEEQUIP) to classify three disability statuses setting ‘no disability’ as a reference. Respondents who answered ‘yes’ to the questions regarding whether they have limitations in performing activities and use special equipment were categorized into the ‘Yes, equipment needed’ group. Individuals who reported having limitations in performing activities but did not report using special equipment were categorized into the ‘Yes, no equipment needed’ group and individuals who answered ‘no’ for both questions were coded as the reference group (no disability). Individuals who responded that they have no limitations but use equipment were treated as missing data.
For smoking status, individuals who answered as current non-smokers were set as the reference group.
BMI respondents were classified into 3 BMI categories. Those with BMIs less than 25.0 were categorized as normal weight or underweight, those with BMIs between 25.0 and 29.9 were categorized as overweight, and those with BMIs greater than or equal to 30.0 were categorized as obese. Value 9 (Don't know/Refused/Missing, Notes: _BMI4=9999) were coded as 0.
For health insurance status, respondents answered the question “Do you have any kind of health care coverage, including health insurance, prepaid plans such as HMOs, or government plans such as Medicare?” Those who responded ‘yes’ were classified as individuals with health insurance and those who responded ‘no’ were classified as individuals without health insurance. A ‘don't know/not sure’ response was considered a nonresponse. Subjects who classified as having health insurance were used as the reference.
Selected socioeconomic variables were adjusted in the models including race, education, sex, and marital status. Individuals who responded ‘don't know/not sure/refused’ to the race questions were classified as ‘other’ in our analysis. We identified individuals as having a high school degree or higher as the reference group. For sex, ‘male’ was used as the reference group. For marital status, we assigned only those who responded as ‘married’ to the married group and the rest of the respondents (divorced, widowed, separated, never married, and a member of an unmarried couple) to the unmarried group. Unmarried was used as the reference group. Respondents who refused to disclose their marital status were treated the same as missing. All variable, except income, operationalization was performed following the classification scheme of McGee and Thompson [2] for the purpose of comparing the results for individuals in the same age group.
Annual household income was classified into 5 categories, including less than $15,000, $15,000 to less than $25,000, $25,000 to less than $35,000, $35,000 to less than $50,000, and $50,000 or more. Since this variable is excluded from the final model due to multicollinearity issue (more details explained in the discussion part), the missing value of income variable is not deleted from the whole sample.
3. Analyses
Analysis of sample frequencies and weights was performed to compare the distribution of selected variables in each group. Then bivariate analyses were conducted to identify the statistical significance of each variable related to the outcome variable of interest. Multivariable logistic regression was used to calculate odd ratios. Three logistic regression models were fitted to the data to examine the relationship between depression and unemployment while adjusting for age and other confounding variables. First, we performed a logistic regression including age categories (18~25; 26~41; 41~60; 61~65) to examine whether age is associated with depression risk when controlling for socioeconomic and health insurance variables. In the second model, we added disability status to the analysis to see whether disability status affects the relationship. The last model adjusted for smoking and BMI in addition to the sociodemographic, health insurance, and disability variables. Finally, we compared the odds of depression between unemployed and employed people in different age groups. The analyses were completed using weighted data to account for the complex sample with STATA (version 14.2).
|
RESULTS
|
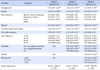
The overall sample comprised of n=53,406 individuals, of whom 2,546 (7.8%) were identified as being depressed and 3,448 (10.6%) were unemployed. Overall the sample had more females (n=18,864, 57.8%) and more individuals with a race identification of White (n=23,975, 73.4%). The majority of respondents had received a high school degree or higher (n=30,994, 94.9%), claimed no disability (n=27,323, 83.7%), and were non-smokers (n=26,238, 80.3%). Individuals in the younger age group (18~25 years; n=2,673) were less likely to be married (n=237, 16.4%), less likely to have health insurance (n=485, 33.6%), and more likely to have normal weight (n=386, 26.7%) or be underweight (n=740, 51.3%) compared to individuals in the older age groups. Depression rates and unemployment rates were highest in the18~25 age group; 12.3%(178) were identified as having depression and 22.5%(325) were unemployed (Table 1).
|
1. Bivariate Analysis
The bivariate relationships between potential confounders and depression as well as unemployment in sample of all ages together were calculated with χ2 analyses. In bivariate analyses, depression was significantly associated with other independent variables (Table 2). Females were more likely to report depression (9.2%) compared to males (5.9%) (p<.001). Black or African Americans (9.9%) were more likely to be depressed compared to White (7.4%), Hispanic (9.2%), and other races (7.1%) (p<.001). About 17.8% of adults without a high school degree reported depression compared to 7.3% of those with at least a high school degree (p<.001). Those unmarried (11.8%), without health insurance (15.5%), or reporting a disability and needing equipment (28.4%) were more likely to report depression compared to their respective reference groups (p<.001). Smokers (16.3%) were more likely to be depressed than nonsmokers (5.7%) (p<.001). BMI was also related to depression. 10.6% of respondents classified as obese reported depression, which was significantly more than those who were categorized as overweight (6.6%) and normal weight or underweight (6.5%) (p<.001). Finally, 12.3% of respondents aged 18 to 25 reported depression, 8.8% of 26 to 40 year-old respondents reported depression, 7.7% of 41 to 60 years old respondents reported depression, while 4.4% of respondents aged between 61 to 65 reported depression.
|
Being unemployed was also associated with other independent variables. Blacks or African Americans (18.4 %) were significantly more likely to report being unemployed compared to Hispanics or Latinos (13.6%), other races/ethnicities (12.1%), and Whites (8.5%) in all age groups (p<.001). Those without a high school degree (27.4%), unmarried (16.2%), or without health insurance (30.0%) were more likely to report being unemployed compared to their respective reference groups (p<.001). Additionally, 19.3% of smokers reported being unemployed compared to 8.4% of nonsmokers (p<.001). Those reporting a disability and needing equipment (27.6%) were more likely to be unemployed compared to those with a disability but not needing equipment (18.5%) and those without a disability (8.8%) (p<.001). 12.1 % of obese respondents reported unemployment, which was significantly more than those who were categorized as overweight (9.4 %) and normal weight or underweight (10.3%) (p<.001). Finally, 22.5% of respondents aged 18 to 25 years reported being unemployed, 10.7% of those aged 26 to 40 years reported being unemployed, and 9.7% of those aged 41 to 60 years reported being unemployed, while only 9.9% of respondents aged 61 to 65 years reported being unemployed.
2. Multivariable Analysis
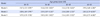
Multivariable logistic regression was used to calculate odd ratios and three logistic regression models were fitted to the data to examine the relationship between depression and unemployment while adjusting for age and other confounding variables (Table 3). There was a clear trend in the odds of depression in all age groups when adjusted for unemployment and other variables. In all three models tested, we found that individuals in the older age group (aged 61~65) have a lower depression risk compared to the younger age group (aged 18~25) after adjusting for other variables including being unemployed. This can be interpreted as older people being less likely to be depressed than younger people when controlling for risk factors like unemployment, together with other demographic and health variables.
|
We then compared the relationship between depression and unemployment in different age groups (Table 4). We found that unemployment is associated with depression in all age groups, but different age groups have different scales of association. In model 1, the odds of depression were 3.14 (95% CI: 2.58~3.82) times higher for unemployed respondents aged 26~40 compared to employed people in the same age group. In models 2 and 3, the odds of depression were 2.5 times higher for unemployed respondents compared to those employed in this age group. For the age group of 41 to 60 years old, the odds of depression were 3.16 times higher (95% CI: 2.74~3.65) for the unemployed compared to those employed in model 1, whereas in model 2 and 3 the odds were 2.34 and 2.16 times higher, respectively. For respondents aged 61~65, the odds of depression were 3.95 (95% CI: 2.48~6.28) times higher for unemployed people in model 1, and 2.81 times higher in models 2 and 3. In other words, respondents in the 61~65 years old age group exhibited the highest increased risk of depression when unemployed.
|
To summarize, the initial analysis indicates that the older the age group, the lower the odds of depression after adjusting for employment and other confounders (Table 3). However, when comparing models by age group, we found that individuals in the older age group had higher odds of depression if they were unemployed compared to employed individuals (Table 4). This could suggest that older people who are unemployed have a higher risk of depression than individuals who are unemployed in younger age groups.
|
DISCUSSION
|
This study aimed to explore the relationships between employment status, depression, and age. The results demonstrate that there is an association between unemployment and depression which differs in magnitude by age group. The findings show that unemployed older adults are more likely to experience depression than unemployed younger adults. There are potential socio-economic reasons underlying these differences as well as the clinical and policy implications of the findings that merit further discussion.
Although younger adults reportedly experience higher unemployment rates than older adults, their socio-economic burden seems less than other age groups, thus exhibiting lower odds of depression compared to other age groups. Younger adults may experience comparatively a lighter economic burden due to less expensive health insurance costs and shorter unemployment periods. In contrast, older adults carry the burden of having to pay for their increasing health insurance costs related to multiple chronic conditions while finding new employment can be more challenging compared to younger adults in their job search [14, 15, 16]. In particular, the economic burden for those under 65, who do not yet qualify for Medicare benefits in the US, may peak a few years before turning 65 due to high insurance costs [16]. According to Smolka and colleages [16], adults ages 50 to 64 face rising out-of-pocket costs for health care and declining access to employersponsored health coverage. Moreover, average annual premiums for private health insurance were the highest for the age group 60~65 (18% more than for age 55~59 and 93% more than for <65)[16]. In our study, health insurance status was a significantly associated factor with depression and we controlled for this factor in all three of our models, but the socio-economic status related to health insurance or unemployment were not examined in more detail due to data limitations.
Another aspect to consider regarding economic burden is the period of unemployment. Older workers' unemployment is mainly characterized by difficulties in finding a new job for those who have lost their jobs [14]. Workers 45 and older who have lost their jobs often encounter difficulties in finding a new job [15]. In our study, we examined unemployment periods (less or more than 1 year) by age group and found that older adults had similar rates of unemployment for shorter and longer periods (4.0% for less than 1 year and 5.9% for more than 1 year), whereas unemployment periods for young adults were often shorter (13.4% for less than 1 year versus 9.1% for more than 1 year). Thus, the potential difference in the degree of economic burden and depression experienced by older adults may be explained by differences in length of unemployment.
We also tested income variable but excluded it from the final model based on the following reasons we get from adding the variable into the model. First, in a general sense, income is highly related to employment status. Second, adding income to the model make the relationship between depression and unemployment less significant. Third, adding income does not increase the goodness of fit of the model and decreased the power of the model. In this way we think income may be a partial mediator between unemployment and depression and excluded income from our final model.
Previous studies exploring the association between unemployment and depression among older adults around the world have reported mixed results [9, 10, 17, 18, 19]. One study performed in Taiwan found that among Asian older adults late-career unemployment (defined as age between 50~64) was associated with increased all-cause mortality and functional disability, but was not statistically significantly associated with depression [3]. Another study from Germany reported significant association between longterm unemployment and minor depression in older adults, affecting almost 16%(n=35) of the study participants [20]. Although we controlled for race and ethnicity in our study, the above findings suggest that race/ethnicity may still contribute to the association between unemployment and depression in older adults. Further research exploring these relationships, particularly for the age group between 61~65 prior to eligibility for Medicare benefits, is much needed.
In interpreting the associations identified in the present study, we also need to take into account potential mediating or moderating clinical factors. Many previous studies have reported an association between unemployment and incidence of cardiovascular diseases and mortality, even after adjusting for confounding factors such as smoking, alcohol consumption, dietary intake, obesity, hypertension, dyslipidemia, and diabetes [21, 22]. Studies have identified a two-way relationship between cardiovascular diseases and depression, indicating that at least a quarter of cardiac patients suffer with depression, and adults with depression often develop heart disease [23, 24]. Considering older adults are more likely to live with various health challenges, these challenges may be a potential mediating or moderating link between unemployment and depression. While our models incorporated and controlled for some key health status data made available through the BFRSS such as smoking, obesity, and disability, these factors do not comprehensively capture potentially relevant health conditions.
In many respects the most straightforward implications of the age group differences of impact of unemployment on depression is with regard to the allocation of available resources to support the vulnerable groups. According to the Society of Adolescent Health and Medicine, over 30 mental health resources including online resources, support groups, peer networks, helplines, treatment locators, and advocacy opportunities from the government or non-profit organizations are freely and readily available to young adults aged between 18~25[25]. In contrast, mental health support for older adults before retirement is scarcer. The National Institute of Mental Health provides around 10 resources for older adults, including federal resources and hot lines in the US [26]. Therefore, more policies to address depression experienced by older adults should be developed.
In addition, the results of studies exploring the relationships between age group variation, unemployment, and depression may aid the clinical recognition of depression among older adults. Clinicians can be alerted to the presence of a high odds of depression for unemployed people within an age group that might otherwise have been overlooked in prevention or treatment due to many other emergent health concerns. Five top priority intervention areas for healthy aging from the World Health Organization Regional Office for Europe focus more on physical aspects of health such as preventing falls and promoting physical activity, while mental health issues are not emphasized [27]. In the US, optimizing physical, cognitive, and mental health was one of the goals for healthy aging from the U.S. Department of Health and Human Services [28], but these goals were formulated targeting mostly 65 and above individuals with Medicare coverage, leaving 61~65 adults who do not qualify for Medicare benefits outside this scope. Mental disorders are often not considered as priority conditions to deal with by clinicians or patients. The findings of this study may serve as an alert to both clinicians and patients.
1. Limitations
There are other limitations of the BRFSS to be considered in interpreting and generalizing the findings. First, as discussed by McGee and Thompson [2], the current study results might be skewed because of the potential undercoverage of emerging adults in the BRFSS, as many of them use cellular telephones instead of landlines [29]. Second, as this study was designed to extend the earlier findings of McGee and Thompson [2] by identifying possible age group differences, there were some limitations in variable selections. Lastly, the PHQ-8 questions were an optional module and only 12 states asked these questions in 2010. Therefore, the results are limited to respondents from those 12 states.
In addition to the limitations from BRFSS, there are other possible limitations from using survey data. Like most survey data, this study has limitations related to the selfreported symptoms of depression as well as other covariates. Additional social and clinical information such as income, behavioral observation, medication history, and a formal depression diagnosis would increase the precision of the study.
How age groups are divided could also yield different magnitudes of the associations between unemployment and depression in each age group. We used preferred terms for age groups from Academic Search Premier & SocIndex to divide age groups as the groups are based on developmental tasks, not merely on 5- or 10-year age brackets. In addition, the younger adult age range exactly corresponds to the range used in McGee and Thompson [2] thus enabling comparison of their results with the results of our study. Further research exploring the relationship using variations in age groups is recommended.
|
CONCLUSION
|
It is critical for policy makers and professionals to extend consideration of the impact of unemployment on mental health to older adults. Most literature to date has focused on younger adults, as they have higher rates of unemployment and are thought to be more prone to experiencing depression in response to becoming unemployed compared to their older counterparts. However, the results of our study reveal that when older adults are unemployed, they actually exhibit higher odds of experiencing depression (once other confounding factors are taken into account) than younger adults. Thus decision-makers should ensure that mental health resources are available to address the needs of older adults experiencing unemployment.
|
Notes
|
This research was supported by the Comparative and Cost-Effectiveness Research(T32 NR014205) and Reducing Health Disparities Through Informatics(T32 NR007969) training grant through the National Institute of Nursing Research.
|
References
|

 KACHN
KACHN




 Cite
Cite