Articles
- Page Path
- HOME > Res Community Public Health Nurs > Volume 34(4); 2023 > Article
-
Original Article
- Experience Related to Acceptance of Illness among People with Early-Stage Dementia: A Phenomenological Study
-
Jaewon Park

-
Research in Community and Public Health Nursing 2023;34(4):241-254.
DOI: https://doi.org/10.12799/rcphn.2023.00157
Published online: December 29, 2023
Assistant Professor, Department of Nursing, Hannam University, Daejeon, Korea
- Corresponding author: Jaewon Park Department of Nursing, Hannam University, 42, 70, Hannam-ro, Daedeok-gu, Daejeon 34430, Korea Tel: +82-42-629-8478, Fax: +82-42-629-8480, E-mail: jwpark@hnu.kr
Copyright © 2023 Korean Academy of Community Health Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0) which allows readers to disseminate and reuse the article, as well as share and reuse the scientific material. It does not permit the creation of derivative works without specific permission.
- 1,316 Views
- 53 Download
Abstract
-
Purpose
- This study aims to describe the structure of the experience related to acceptance of illness among people with early-stage dementia (PWED).
-
Methods
- Participants were six people who had Alzheimer’s disease or vascular dementia. Their clinical dementia rating scores were 0.5 or 1. Data were collected from individual in-depth interviews. The collected qualitative data were analyzed based on Giorgi’s descriptive phenomenological method.
-
Results
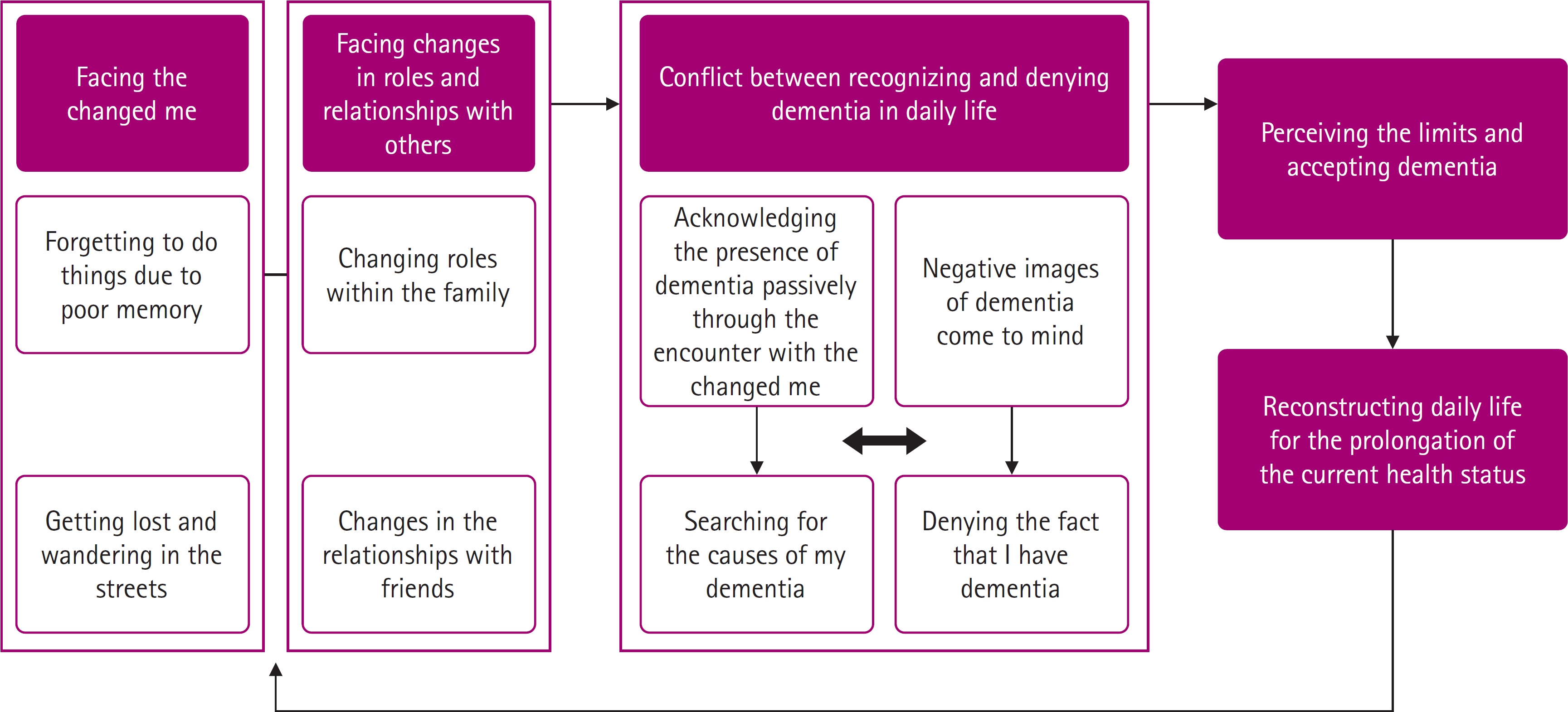
- The five constituents and eight sub-constituents were derived from the experience related to acceptance of illness among PWED; ‘Facing the changed me’, ‘Facing changes in roles and relationships with others’, ‘Conflict between recognizing and denying dementia in daily life’, ‘Perceiving the limits and accepting dementia’, and ‘Reconstructing daily life for the prolongation of the current health status’.
-
Conclusion
- This study contributes to the expansion of the in-depth understanding of the experience related to acceptance of illness among PWED. The results of the study will be helpful as basic data for community health nurses to develop interventions to improve acceptance of illness of PWED.
- Dementia is a clinical syndrome characterized by cognitive decline, and it is caused by various causes, including Alzheimer’s disease and vascular dementia [1,2]. Since dementia causes a decline in cognitive functions including memory, a decline in the ability to perform activities of daily living (ADL), changes in emotions and behaviors, and limitations on social participation [1], it is a major cause of disabilities and dependence in daily life in elderly people [1]. Currently, the international community is paying attention to dementia due to the increase of the number of people with dementia as a result of the growth of the elderly population [1]. Many countries around the world are making efforts for the improvement of quality of life among people with dementia as well as the prevention, treatment, and management of dementia [3].
- Dementia can be divided into early, middle, and late stages according to the levels of cognitive function, the ability to perform ADL, and independence [4]. People with early-stage dementia (PWED) are able to perform ADL relatively independently, compared to those with middle-stage or late-stage dementia [4]. But due to progressive cognitive decline, they experience the gradual functional decline in the ability to perform daily activities and their roles in daily life, limitations on participation in social activities, and the gradual reduction of control over behavior [5,6]. Moreover, unlike other chronic diseases, dementia is characterized by the cognitive decline that precedes a decline in physical function [4]. For this reason, PWED experience greater confusion due to changes in their daily life resulting from cognitive decline rather than physical health problems [4]. They tend to think their confusion results from some other problem and attempt to fix the situation rather than regarding their symptoms as the symptoms of a disease [4].
- Acceptance refers to recognizing and actively accepting a situation rather than changing the situation, when an individual is put in a situation that may pose a psychological threat to the person [7]. Since acceptance leads individuals to actively accept what they are experiencing as it is rather than making unnecessary judgements about the current feeling, thoughts or emotions [8], it has therapeutic effects regarding the enhancement of quality of life. For this reason, this aspect of acceptance has been applied in health-related fields [9]. Acceptance of illness means accepting disease as well as the reality related to disease, including negative thoughts, emotions, and changes caused by disease [10]. Research on acceptance of illness has been conducted in relation to various chronic diseases, such as cancer [10,11], heart failure [12], diabetes [13], chronic respiratory disease [14], end-stage renal disease [15], and chronic pain [16]. According to the results of previous studies, acceptance of illness reduces psychological pain and distress as well as anxiety and depression in patients [10,11,13,15], and influences the physical, emotional, and social functions of patients [12]. These findings indicate that acceptance of illness is closely related to the quality of life of patients [12-15]. Although acceptance of illness has important meaning for patients with chronic diseases [12], among previous studies on dementia, only one study [17] reported that emotional adaptation to disease is one of the major attributes that determines the emotional well-being of people with dementia. Moreover, it is difficult to find studies that conducted an in-depth exploration of acceptance of illness in people with dementia.
- Until the 1980s, research on dementia was based on the biomedical perspectives that conceptualized dementia as neurological damage [18], and these studies of dementia based on biomedical perspectives brought about the development of pharmaceutical interventions [19]. However, biomedical perspectives are focused on the functional loss and decline of people with dementia and the experience of caregivers [2,18]. Therefore, some researchers pointed out the limitation of biomedical perspectives in that they cannot sufficiently explain dementia [19-21]. Subsequently, research on dementia has been gradually expanded to the perspectives that acknowledge the importance of the psychosocial factors, humanity, experiences, and well-being of people with dementia [2,18-21]. Recently, person-centered care has been emphasized, and the concept of person-centered care was proposed by Kitwood [22,23]. Kitwood [22,23] also regarded people with dementia as beings with subjectivity and psychosocial needs, and maintained that it is necessary to explore their experiences. Some researchers raised questions about the reliability of the reports of people with dementia who have cognitive impairment [21]. However, in recent years, social consensus has been largely reached regarding the view that the essential nature of experience should be explored from the perspective of people with dementia who directly experience the phenomenon [21]. Further, the World health organization (WHO) also suggests that when researchers attempt to understand vivid experiences related to dementia, it is imperative to investigate the phenomenon through people experiencing dementia [1]. As a result, qualitative research on the self-reported experiences of people with dementia has been increasing.
- Previous studies on the experience of people with dementia explored the following experiences related to dementia: the experiences of living with dementia [5,24], shame and loss [6], adaptation to dementia symptoms [25], strategies for coping with dementia symptoms [26], and experiences of dementia diagnosis [27]. In addition, some previous studies conducted the synthesis of the findings of primary qualitative studies on the experiences of people with dementia, and these studies analyzed qualitative findings mainly focused on relationships [28], lived space [29], lived time [30], or coping strategies [31]. There were also studies that conducted the synthesis of the experiences of dementia diagnosis [32,33]. However, there have been few studies to explore the experience of acceptance of illness among people with dementia, so there are limitations on gaining an understanding of the experience. Nevertheless, acceptance of illness is important for PWED because it helps them to get used to limited independence and increasing dependence on others in daily life due to the disease [14], and it contributes to the reduction of pain and distress related to various changes caused by dementia [10]. Furthermore, PWED tend to think that there is something wrong and struggle to fix the situation rather than accepting dementia, but at the same time, they want to know how to adapt to changes occurring together with the disease [4]. Based on the findings of prior studies described above, acceptance of illness should be viewed as a prerequisite for the improvement of quality of life among PWED, and there is a need to explore the experience of acceptance of illness from the perspective of people with dementia prior to the development of interventions or strategies for acceptance of illness among PWED.
- Therefore, this study attempted to explore the experience of acceptance of illness in PWED by applying the descriptive phenomenological method proposed by Giorgi [34,35]. On the basis of Husserl’s phenomenology [35-37], Giorgi proposed a phenomenological method for exploring the fundamental nature of the experiences that individuals go through in the world of everyday life [35,37]. Based on Husserl’s epistemology, Giorgi claims that insubstantial phenomena, such as dreams, hallucinations, and memory, are experienced through individuals’ consciousness [35], and thus he emphasizes qualitative research as a method for gaining knowledge about empirical phenomena [35]. In addition, according to Giorgi’s descriptive phenomenological method, researchers should concentrate on participants’ statements themselves and the meanings of the statements rather than the truthfulness or falsity of the statements [34], and describe participants’ experience in a detailed and concrete manner [35]. In this way, Giorgi’s descriptive phenomenological method presents a method of qualitative research and phenomenological research without resorting to biomedical models and the paradigms of natural sciences based on empiricism [36], and it allows researchers to focus on the subjects of experience and their experiences [34,35,38]. In this respect, Giorgi’s phenomenological approach provides validity for the inquiry of the experiences of people with dementia.
- This study aimed to explore the structure and meaning of the experience of acceptance of illness in PWED by applying Giorgi’s descriptive phenomenological method [34,35]. Through this inquiry, this research sought to present a deeper understanding of the experience of acceptance of illness in PWED and the results of this study are expected to contribute to presenting a theoretical basis for the development of nursing practice and interventions for helping PWED to accept their dementia more actively.
Introduction
- 1. Study design
- This study is a qualitative research to investigate the structure of the experience of acceptance of illness in PWED by applying a phenomenological method.
- 2. Participants
- The participants of this study were people with early-stage dementia registered at a dementia care center located in Seoul. Initially, participants were selected by the following inclusion criteria: (1) a diagnosis of Alzheimer’s or vascular dementia; (2) a Clinical Dementia Rating (CDR) of 0.5 (suspected dementia) or a CDR of 1 (mild dementia). In addition, to select participants who can give an account of their experience in a psychologically stable condition, participants were limited to people who were diagnosed with dementia at least 6 months ago. People diagnosed with dementia at least 6 months ago were recruited because a previous study [39] reported that people who were diagnosed with dementia less than 6 months ago patients are at high risk for suicide due to a high level of stress and emotional pain caused by dementia diagnosis. Those who had difficulty communicating verbally due to other physical diseases or were diagnosed with psychiatric diseases were excluded. Participants were selected by a purposive sampling method from elderly people who were using a dementia care center, understood the purpose of this study, and gave consent to data collection. More specifically, the people who met the inclusion criteria of this study and were judged to be able to understand and adequately answer the questions of interviews were recommended by the person in charge of the cognitive rehabilitation program. A total of six people were recommended, and the researcher met them individually, and gave them explanations about the researcher, the purpose of the study, the method of research participation, and the reason why they were recommended as participants. All of the six people fully understood the researcher’s explanations, and voluntarily agreed to participate in the study, so they were all selected as participants.
- 3. Data collection
- Data was collected through individual interviews with the participants by the researcher from October 14, 2015 to April 5, 2016. All of the six participants completed interviews without dropping out or refusing to participate. Interviews were conducted on the days when the participants visited the dementia care center to participate in the cognitive rehabilitation program. Each interview lasted for one hour or for one and a half hour, and two or three interviews were performed for each participant depending on participants. For the interview location, interviews were conducted in the education room or the interview room of the dementia care center that the participants used every week to ensure that participants would feel comfortable during interviews and respond to interviews in a natural situation. Interview guidelines created in advance were used to prevent omitting questions during interviews and proceed with interviews in a natural manner. The interviews were recorded using a recording device, and the participants’ non-verbal messages observed by the researcher during the interviews as well as the researcher’s impressions about the participants and their statements during the interviews were recorded in interview notes.
- The researcher started interviews with participants using questions about common topics such as the weather, their mood, and their special experiences during the past week. The order of the questions was flexibly changed according to the flow of the conversation to ensure natural interviews. During the first interview, participants were asked questions about their general characteristics, such as gender, age, the type of dementia, time elapsed since dementia diagnosis, and the presence of other diseases, and the conversations about these questions were helpful in leading conversations about dementia naturally during the interviews. According to the descriptive phenomenological method suggested by Giorgi[35], to explore the essential nature of the experience of acceptance of illness by using the research question “Please tell me about the situations related to the experience of accepting the disease called dementia in your daily life”, specific interview questions were designed to elicit narratives about the essential elements of experience, such as the subject of experience, the experienced object, temporality, spatiality, relationships between oneself and others, the meaning of life for the subject, and value judgements of the subject [37] (Table 1). The researcher transcribed recordings within 3 days from the date of data collection, and tried to exactly transcribe what participants said by comparing the content of recordings with transcripts. Any matters requiring additional confirmation were included in the questions of the subsequent interview, and data collection was conducted until data saturation was reached.
- 4. Data analysis
- Data analysis was conducted along with data collection in a cyclic manner, and carried out according to Giorgi’s descriptive phenomenological method [34,35]. Prior to data analysis, the researcher’s assumptions and preconceptions about PWED, which were formed based on previously obtained knowledge and experiences, were described and revealed. The researcher had the following assumptions and preconceptions about PWED: ‘PWED probably tried to deny their situation when they were given a dementia diagnosis’; ‘PWED will have anxiety and fear about the progress of the disease’; ‘All the thoughts and behaviors of PWED will be focused on dementia after dementia diagnosis’; and ‘PWED will try to avoid expressing or disclosing anxiety about the possibility of their disease getting worse to others.’ If the assumptions and preconceptions of the researcher are involved in data analysis, they interfere with the exploration of the essential nature of experience. Therefore, in the process of data analysis, the researcher made a conscious effort not to allow the researcher’s assumptions and preconceptions to influence data analysis by writing them down and bracketing them [35].
- In the first phase of data analysis, to obtain an understanding of the overall content of the statements of participants, the researcher was immersed in the situations described by participants and repeatedly read transcripts until the researcher gained a clear perception of the overall experience of participants. In the second phase of data analysis, classification of meaning units from an academic perspective was performed. The researcher slowly read the statements of participants from a perspective of nursing science, and indicated the parts showing changes in meaning using underlines and parenthetical marks and wrote brief memos about the essential element of experience that particular statements constituting a meaning were related to. A total of 195 meaning units were finally derived through several repeated analyses and checking processes. The third phase of data analysis is the stage of transforming meaning units into academic terms. Starting with the first transformation process of changing meaning units expressed in the first person into third-person expressions, the transformation of meaning units into academic terms was performed a total of six times through reflection and free imaginative variation. In terms of validity, the process of transforming meaning units into academic terms, the process of deriving constituents, and the final results were reviewed by 3 experts in the field of nursing who were well versed in qualitative research methods and research on dementia. The fourth phase of data analysis is the stage of describing the structure of experience. In this stage, the finally transformed meaning units and constituents were compared and contrasted from an integrated perspective, and they were described by synthesizing them into a single structure about the experience of acceptance of illness of PWED. The descriptions of the structure of experience were revised a total of three times. Each time they were revised, they were reviewed by 5 experts in the areas of qualitative research and research on dementia.
- 5. Research preparations
- The researcher completed a course on qualitative research methodology as part of doctoral coursework, faithfully carried out preparations as a researcher in qualitative research through opportunities for studying and practicing qualitative research methods, including participation in academic conferences and seminars, and published research papers applying qualitative research methods in academic journals. The researcher has also been continuously making efforts to expand theoretical sensitivity to dementia and people with dementia by continuously conducting research on dementia and practical guidance for undergraduate courses implemented in nursing homes. In addition, the researcher participated in the process of tests for diagnosing dementia for 6 hours a week for about 6 months with the permission of the director of the dementia care center, who gave approval for data collection. This process served as a training process for the researcher to increase an understanding of the symptoms and responses of people with dementia, elicit in-depth accounts from participants during interviews, and naturally maintain the flow of interviews by flexibly responding to the reactions of participants. Additionally, the researcher participated in the cognitive rehabilitation program and the exercise program for 1 hour per week for 4 months with the permission of the director and the person in charge of the cognitive rehabilitation program of the dementia care center. This process helped to narrow emotional distance and form a mutual trust relationship between participants and the researcher.
- 6. Ethical considerations
- This study was conducted after obtaining approval from the Institutional Review Board of Korea University (1040548-KU-IRB-15-181-A-1). In this study, the following efforts were made to adhere to research ethics. First, considering participants’ poor memory, they were reminded of interview appointments a few days before conducting interviews in order to reconfirm interview appointments and their consent to research participation. Second, participants were given explanations about the researcher, the purpose of the study, the reason they were recommended as participants, recording interviews, how to store the research data, protection of confidentiality and anonymity, and their right to refuse to participate or withdraw from research at any time without any disadvantages. Then, it was checked whether they understood the explanations about research by asking them about the content. After it was confirmed that they understood all the important matters regarding research participation and voluntarily agreed to participate, written informed consent was obtained from them, and then interviews with them were conducted. Third, during the interviews, participants were asked one question at a time in easy-to-understand and concrete language expressions, and they were given sufficient time to answer. In addition, when participants were having trouble finding right words or expressions, clues for them or expected words were given so that they could participate in the interview without feeling frustrated. Fourth, even when participants repeatedly say the same thing or gave a wrong or illogical response to a question, the researcher listened to what they said until they finished talking without interrupting them. Lastly, while conducting the interviews with participants, the researcher paid attention to whether they felt tired or their state of mind in the process of the interview, and a small amount of money was paid to the participants as a token of appreciation.
- 7. Ensuring the quality of research
- To ensure the quality of research, evaluation criteria proposed by Lincoln & Guba [40] were applied. First, to ensure the credibility of the study, the researcher tried to gain a sufficient understanding of participants and form a trust relationship with them by participating in tests for diagnosing dementia, the cognitive rehabilitation program, and the exercise program for several months prior to data collection. On the other hand, according to Giorgi’s descriptive phenomenological method, research results are derived based on the researcher’s academic perspective, and the experiences and meanings derived from an academic perspective are different from the raw experiences and meanings as experienced by the participants, and thus it has been suggested that it is not appropriate to confirm research results through participants [41]. Therefore, in this study, the process of confirming research results with participants was not conducted. Instead, to make up for this omission of the process of checking research results with participants, participants were asked the same question two or three times by expressing it in different ways, and it was checked whether their responses were consistent in order to ensure the authenticity of collected data. Data saturation was ensured by finishing interviews when it was confirmed that new information was not derived any more for each participant during the second or the third interview depending on individual participants.
- To secure transferability, participants were selected by a purposive sampling method, questions were created to reveal the essential elements of experience, and the researcher tried to sufficiently describe the experience of acceptance of illness of PWED from an integrated perspective through faithful immersion in the statements of participants. In addition, to secure dependability, during the processes of data collection and analysis, the researcher recorded the processes performed and rational bases for them by writing research notes, and conducted an external audit by getting the content of research notes reviewed by a fellow researcher who had the experience of qualitative research and did not participate in this research. Additionally, to secure confirmability, the researcher’s assumptions and preconceptions about PWED were disclosed in advance by describing them, and the researcher tried to prevent them from intervening in this study during the entire process of research. In addition, to confirm whether research results were derived based on collected data without any interventions of the researcher’s preconceptions, an external audit for the research process and results was conducted by experts well versed in qualitative research methods and research on dementia.
Methods
- The general characteristics of the participants are shown in Table 2. The core themes of the experiences of acceptance of illness in PWED were derived as five constituents and 8 sub-constituents. The five constituents of the experience of acceptance of illness in PWED were as follows: ‘Facing the changed me’, ‘Facing changes in roles and relationships with others’, ‘Conflict between recognizing and denying dementia in daily life’, ‘Perceiving the limits and accepting dementia’, and ‘Reconstructing daily life for the prolongation of the current health status.’ The results of this study showed that the participants were not able to do what they needed to do because of poor memory, and were faced with the experience of finding themselves getting lost and having difficulty finding their way around familiar spaces, the changed roles of themselves and their family members, and changes in the relationships with friends. In particular, as they were faced with their changed selves, they could not help but agree that they had dementia. Also, they looked back on their past life in search of the causes of their disease, and when they found the causes of their dementia, they acknowledged that they became dementia patients. Meanwhile, participants got to think about the nature of dementia, and it occurred to them that as far as they knew, dementia is a disease that make people behave unpredictably and irrationally, causes pain to the family, and imposes a huge burden on the family. Then, in light of the fact that they did not show such behavioral symptoms of dementia, they could not acknowledge the fact that they had dementia. In this way, participants experienced a tight conflict between the recognition and denial of dementia within themselves. However, since participants knew that dementia progressed with time and would continue to progress, they realized their limits and accepted the fact that they were dementia patients. In addition, they filled their daily life with healthy lifestyle and efforts to prevent or delay memory decline in the hope that they could slow down or stop the progress of dementia and maintain their current health status (Figure 1).
- Constituent 1. Facing the changed me
- The participants came to have difficulty continuously remember some information and recalling it. They found that the flow of thoughts was not maintained due to poor memory. They found themselves frequently forgetting to do what they had to do because the connection between thought and action was previously naturally achieved without any efforts but was now disrupted by poor memory.
- “A little bit these days … I now forget things often unless I write them down. Even recently, during Chuseok, we were holding a memorial service for ancestors, I had bought persimmons (for the ancestral rite), but I couldn’t remember where I put them, and I even forgot buying them. However, afterwards, when I opened the door of the refrigerator for kimchi after finishing the memorial service, I found that they were in the refrigerator. Since then, I often get startled whenever similar things happen.” (Participant 1)
- “Now, I can’t remember things, I can’t. I need to, hmm, re-, remember all the things that happened yesterday, but I can’t remember them. I can’t remember things like what I did yesterday. I fail to keep appointments all the time.” (Participant 4)
- The participants found themselves getting lost and having trouble finding their way around the places that they usually frequented or they found themselves standing in a place other than their intended destination. They felt confused when they found it difficult to find their way around familiar places where they had lived so far.
- “That day, I was going alone, … strangely, □□□, I couldn’t find that place. … ‘Uh, this is strange … here, □□□ is only several stops away, why can’t I remember (how to go there)?’ I thought to myself like this, and I stood at a bus station like this. … That man told me, ‘You took the wrong bus, you should have taken the bus on the other side of the street, but because you took a bus here, you couldn’t find the place.’ … I felt confused and frustrated, … ‘Ah, why I suddenly, it’s the path I use every day, why, why can’t I find my way around here like this?’ When I think about that, I feel so upset and frustrated that I feel like I’m gonna die soon, literally. Indeed, this feeling is beyond words.” (Participant 3).
- Constituent 2. Facing changes in roles and relationships with others
- The participants realized that other family members got to take over their roles that they had performed so far in the daily life of the family. In addition, on the basis of the reduced functional abilities of the participants, their family members restricted or intervened in the things they had done independently, which led to conflicts between the participants and their family members.
- “For me, now, my seals, my bankbooks, and my money and other things in the bank, all the financial matters, my wife manage and take care of them. … And my daughter came and said to me several times, ‘Let Mom do that, you don’t know anything, but why are you making a fuss? … So, we quarreled or argued a lot” (Participant 4)
- The participants became conscious of the fact that they had dementia, whenever they met their friends. As their friends became aware that the participants had dementia or they noticed the participants’ illness through their changed behaviors, they felt that there were changes in their friends’ attitude toward them. Now, they felt uncomfortable in their relationships with friends, experienced emotional damage, and thus gradually came to avoid meeting their friends.
- “The day after tomorrow, again, I have to go to see my college friends, I haven’t yet decided whether to go there or not. … My old image, the way they saw me in the past, it would be ruined. The thought spoils the fun. … My image they previously had about me seem to be going downhill. I feel upset about that.” (Participant 5).
- “I quit (meeting people) a lot. Because, I have no choice but to, this, now, because I have dementia … When people talk about things like that, I feel annoyed. I feel bad, and i often get upset by what they say.” (Participant 1)
- Constituent 3. Conflict between recognizing and denying dementia in daily life
- When the participants encountered changes in themselves during their daily lives, they could not help but agree that they had dementia. In particular, as they found themselves unable to perform daily tasks smoothly, they had no choice but to acknowledge that they had dementia.
- “The path I walk every day, … I need to walk the same path every day, but strange, strangely enough, I found myself waking in this direction. … The senior welfare center is located there, but I found myself standing on a different path. Oh, my gosh, that’s when I realized. I thought to myself, ‘Oh, my … I seems to have dementia …’” (Participant 3)
- After agreeing to the fact that they had dementia, this acknowledgement led participants to search for the reasons why they developed dementia. The participants looked back on their past life, searching for the causes of their dementia. Then, when they found the cause of their disease in their past life, they acknowledged that they had dementia.
- “Indeed, totally bewildering. Hmm, … I had a lot of hobbies, and I also did all of them earnestly, how did this happen, ah, what did I do, in my life, what did I do wrong? I thought a lot about that. …” (Participant 1)
- “Among my siblings, three of them are still alive, ah, two of them, my second older sister and my eldest brother. These two people are still alive, and they don’t have dementia. But I have dementia. But I, I regret that. I drank a lot. Hmm, …. My brother was a heavy drinker, but he quit drinking when he was young. I almost, I quit drinking when I had some health problems, though. … Because I did so, I drank, that I drank too much, that’s the reason I have this disease, I admit this.” (Participant 5)
- Meanwhile, the participants got to think about what disease dementia is, and naturally, negative images related to dementia occurred to them. For the participants, dementia was regarded as a socially inappropriate state that is manifested as concrete behaviors, such as constantly asking for food even after having a meal, yelling at people, going outside abruptly, and aggression. In addition, they thought of dementia as a disease that causes pain to the family and imposes a burden on the family because of irrational behaviors, and they also perceived it as a disease for which there is no cure but which not lead to death easily.
- “For the people I saw on TV, well, some people run away, hmm, some people give their family a hard time, hmm, just, some woman beats her husband, some people ask for meals, and having just finished a meal, they say they haven’t eaten anything yet. When I see things like that, I don’t like it. I feel uncomfortable. Because of that, so, I know, dementia is, how terrible it is. … So, I get to think about the great trouble the family members would have, how many difficulties they would have” (Participant 3).
- Since they did not show such symptoms of dementia, they would not admit that they had the same condition as dementia. Therefore, they separated themselves from dementia, claiming that their health problems were not related to dementia, and they had a normal healthy state.
- “… When I compare myself with that person, there are moments when I think ‘I am, better than that (person), huh, am I like that?’ I feel like ‘But, I am not like that …’” (Participant 5)
- “Even now, I, things like this math, …. Huh! Ah, things like this, 2, 3, 5, 7, 9, and 2, 4, 6, 8. Well, I got every question right. Ah, this is, the cog-, they do cognitive tests, right? Then, I thought to myself, ‘That is doing a cognitive test’, and I easily write down without hesitation, almost nor- … like a normal person! However, the doctor seems to think that I have the disease.” (Participant 2)
- Constituent 4. Perceiving the limits and accepting dementia
- Nevertheless, participants knew that their health status was gradually getting worse with the elapse of time. They also knew that dementia would keep progressing in the rest of their life. While observing their health status getting worse gradually, participants realized their limits that they could not overcome even by great efforts, and thus they accepted the fact that they had dementia.
- “Ah, indeed, it does progress! This disease is, however hard I, this, I come here, try hard, and take medicine, nevertheless, it is slowly progressing, I think like that. Ah, so, I have accepted it.” (Participant 1)
- Constituent 5. Reconstructing daily life for the prolongation of the current health status
- The participants could not just sit idle helplessly and wait for their dementia to get worse. Therefore, they reconstructed their daily life in the hope that their dementia would progress as slowly as possible or would not get worse any more, and thus they could maintain their current health status. Efforts to maintain healthy lifestyle, repeatedly reminding themselves of the information they need to remember, and training for maintaining current memory capacity, such as recording and checking things, became an important part of daily life for the participants.
- “I really hate doing exercises, but because they say exercises are good for health, because they say they are good for dementia, so I walk for exercise.” (Participant 1)
- “I try to think about things again and again, I try not to forget about things, … when I make an appointment, not to forget that appointment, …, I write it on a piece of paper or in a pocket planner, and like this, I attach it. … So, I always carry a pocket planner with a large size like this.” (Participant 2).
Results
1) Forgetting to do things due to poor memory
2) Getting lost and wandering in the streets
1) Changing roles within the family
2) Changes in the relationships with friends
1) Acknowledging the presence of dementia passively through the encounter with the changed me
2) Searching for the causes of my dementia
3) Negative images of dementia come to mind
4) Denying the fact that I have dementia
- In this study, the experience of acceptance of illness in PWED was found to have a structure with the following sequentially appearing constituents: ‘Facing the changed me’, ‘Facing changes in roles and relationships with others’, ‘Conflict between recognizing and denying dementia in daily life’, ‘Perceiving the limits and accepting dementia’, and ‘Reconstructing daily life for the prolongation of the current health status.’ However, in the experience of acceptance of illness in PWED, five constituents do not always occur sequentially in one direction, but the experience has a cyclic structure in which PWED perceive their limit and accept dementia, also engage in the reconstruction of daily life to maintain their current health status, meanwhile, face the changed ‘me’ and changes in their roles and relationships with others once again, and thus experience the conflict between the recognition and denial of dementia again. A study on patients with chronic pain [16] also found that the participants who once accepted their pain returned to the state of non-acceptance, and that pain acceptance is a continuous and dynamic process that requires a long period of time until patients understand and completely accept pain. These research findings show that acceptance of illness cannot be achieved in a short period of time, and it is a task that must be accomplished with patience from a long-term perspective. Therefore, to help PWED to accept their disease, it is necessary to explore methods to help them to accept changes in themselves by gaining an understanding of characteristics and symptoms of the disease, use strategies for responding to changes caused by dementia and maintaining current health status, and at the same time, recognize their dementia more easily and more comfortably. In addition, to help them to accept dementia in a more stable and comfortable manner in the process of perceiving their limit and accepting dementia, it is necessary to take a multidimensional approach including cognitive, psychological and social support from a long-term perspective [16].
- In the first constituent, participants reported facing changes in themselves. More specifically, they found themselves unable to do what they needed to do due to poor memory, and they had the experience of getting lost and not finding their way in a familiar space where they went very often. Dementia patients’ cognitive decline and reduced control over their behavior [6] and their recognition of changes in themselves in relation to limitations on daily activities due to functional declines are common experiences in people with dementia, so they were also reported by other previous studies [5,24]. In addition, changing roles in the family revealed by the second constituent in this study are similar to the findings of previous studies. More specifically, some prior studies [5,24] also reported the experiences of changing roles in people with dementia, such as the experience of decision-making about daily activities that is limited or conducted by other family members and the experience of the transition of roles such as driving to the spouse even though they performed the roles before dementia diagnosis.
- It should be noted that these changes experienced by people with dementia are linked to the loss of independence and the increase of dependence on others [5]. In addition, it is also necessary to pay attention to the finding that it has been shown that although people with dementia show a decline in abilities and functions for ADL, they hope to maintain their daily life autonomously and independently, and further want to be helpful to their family in other ways [24]. Furthermore, people with dementia experience sadness, the decrease of self-confidence, and a reduction in self-esteem due to the loss of independence [5]. Therefore, to help PWED to accept their disease, there is a need to focus on the balance between independence and dependence. For PWED, leading them to adapt to a new way of living by informing them about tools and strategies that can help them to overcome limitations in ADL and perform independent activities will help them to accept changes in daily life. According to a previous study, family members play an important role in helping people with dementia maintaining balance between independence and dependence [16]. Therefore, it is primarily required for family members to understand the feelings and needs of people with dementia regarding changes arising due to dementia. In addition, their family members should try to give people with dementia opportunities to perform daily activities independently, and provide support for them so that they can perform daily activities for themselves if possible. It is thought that such help and support can contribute to the acceptance of illness of PWED because they can increase the family members’ understanding of people with dementia and facilitate family interactions including respect toward each other as shown in a previous study [42].
- In the second constituent of the experience of acceptance of illness, participants reported that they came to avoiding meeting people because they perceived changes in their friends’ attitudes toward them in relationships with friends, and they became uncomfortable about relationships with friends. These results are similar to the findings of some previous studies. For example, a study of people with dementia showed that people with dementia became conscious of others’ gazes or perceptions regarding matters such as how they look to others or whether others already know that they are dementia patients [24]. Also, another previous study of people with dementia found that people with dementia isolate themselves from the world as they become reluctant to go out to avoid others’ negative gazes and sympathy [6]. Based on these findings, it can be inferred that PWED go through internal and external conflicts regarding maintaining their value and others’ respect toward them in their social relationships including relationships with friends [24]. On the other hand, a prior research revealed that while they are trying to hide their symptoms and dementia diagnosis from others, they feel like they are being observed by others, and feel loneliness at the same time [24]. In addition, a prior study reported that people with dementia usually find it difficult to tell others about the sadness and frustrations they experience in the process of struggling to restore daily life disrupted by dementia, and they consider it more difficult to talk about them to friends in particular [24]. In the light of these research results, a warm gaze, understanding, and receptive attitude toward PWED from other people that they encounter in social relationships [9] are considered to be essential elements for acceptance of illness in PWED. Giving help and support to PWED rather than prejudices and stigma toward them will help them to accept their disease because such support would allow them to disclose their disease more comfortably and live in the local community receiving help from others.
- The third constituent of the experience of acceptance of illness showed that there is a tense internal conflict between the recognition and denial of dementia in the participants. In agreement with these results, some previous studies reported similar findings. For example, a previous study described that although people with dementia knew that they had dementia, they denied the fact that they were dementia patients, and avoided using the word dementia [19]. In addition, another prior study reported that when they were faced with a situation when they could not perform daily activities normally, they attempted to avoid the embarrassing situation by resorting to humor or laughing it off and thus separated themselves from dementia [6]. These findings suggest that PWED cannot easily acknowledge the fact that they have dementia even though they have been diagnosed with dementia by a doctor and have been receiving regular checkups and taking medications. This is presumed to be due to the negative social perceptions of dementia. In this connection, as shown in the results of this study, dementia has been described as ‘senility’ or ‘irrational behaviors due to old age’ for a long time, and mass media has depicted dementia with a focus on behavioral and psychological symptoms such as aggressiveness, wandering, hallucinations, and delusion. These misconceptions and inaccurate depictions of dementia have led to the formation of a negative perception of dementia not only among people with dementia but also in the society as a whole. Moreover, negative perceptions of dementia lead people with dementia to regard dementia as a stigma rather than a disease, and thus make it more difficult for them to accept the disease.
- The results of this study showed the tight battle between the recognition and denial of dementia in PWED. According to a previous study of patients with chronic pain [16], patients with chronic pain also experience the conflict between the acceptance and non-acceptance of chronic pain for a long time. These results indicate that patients experience a conflict between the recognition and denial of their disease for a long time. On the other hand, considering a prior study’s finding that a proper understanding of disease is an attribute of disease acceptance [9], it is considered essential for acceptance of illness for PWED to recognize dementia as a disease and have an accurate understanding of dementia. Therefore, nurse should provide continuous education and counselling so that PWED will have a correct understanding of dementia and gain proper insight into the disease, and change their perceptions about dementia into positive and receptive ones [19]. In addition, it is necessary to provide emotional support to PWED while they go through an internal conflict between the recognition and denial of disease. Although policies and campaigns to improve the perceptions of dementia have been continuously implemented at a national level, in order to allow people with dementia to accept dementia more comfortably and live well with dementia, each local community should make more active efforts to build a supportive environment [2].
- In the fourth constituent, the participants realized limitations with the elapse of time, and accepted the fact that they were dementia patients. Similarly, in a study that explored the experiences of patients with terminal cancer [43], acceptance of illness was defined as ‘having to accept’ reality because the participants could not fight and survive their disease. To help PWED to accept their illness, community health nurses are expected to continuously provide them with nursing care including education, counseling, and support. However, especially when PWED accept their illness, nurses need to provide active support and assistance for them so that they will not perceive acceptance of illness as giving up or a crisis. In addition, it is necessary to ensure that acceptance of illness will not be limited simply to the recognition of limitations in people with dementia. In other words, it is necessary to help people with dementia to spend the rest of their life as a meaningful time by finding the meaning of life and looking for and performing things they can do for their family and others for the rest of their life [43].
- Meanwhile, for the participants of this study, time simply meant the progress of dementia, but negative emotions such as fear were not observed. On the other hand, some previous studies [5,24] reported that people with dementia perceived the rest of their life as a fearful time due to the possibility of the complete loss of cognitive function and the uncertainty about how long it would take for their disease to reach the late stage of dementia. In addition, a study revealed that people with dementia considered euthanasia because they feared that they would eventually become ‘a burden’ on their family [5]. Although there are some discrepancies in the research findings of existing studies, for people with dementia, time is considered to have meaning as qualitative time depending on the severity of illness and functional abilities. In other words, in PWED, the quality of time is thought to be proportional to the severity of their illness and inversely proportional to the level of remaining functional abilities. Therefore, if advance care planning, including better disease management plans, plans for the rest of their life, and preparations for death, is implemented together with people with dementia from an early stage of dementia [5], it will not only help PWED to accept their illness but also help people with dementia to arrange the rest of their life and prepare for good death.
- In the final constituent, it was found that participants fill their daily life with efforts to change their lifestyle into healthy ones and the activities of training to prevent memory loss in the hope that they could maintain their current health status. These efforts of people with dementia were also shown by previous studies reporting that people with dementia use auxiliary tools such as calendars, diaries, and tablet PCs, post notes at various places in the house, and try to maintain a positive state of mind [5,24]. Meanwhile, people with dementia want to stay in the community as long as possible [5]. To this end, all the members of the community should provide adequate help to them without any prejudices, and create a community encouraging the participation of people with dementia [5], and there is also a need to develop technologies to support their healthy daily life [1]. This approach is consistent with the change in the international community’s approach toward dementia care from the maintenance of cognitive function and the reduction of behavioral changes in people with dementia to the improvement of quality of life and strategies for living positively with dementia [1]. In a dementia-friendly community [3], PWED are likely to accept their illness more easily.
- The participants of this study were able to express their situations, feelings, and thoughts and even describe their evaluations about themselves and their past life and their hopes for the future. In this respect, it is thought that this study has contributed to the presentation of the feasibility and validity of the research participation of PWED. In addition, through the identification of the constituents of the experience of acceptance of illness of PWED, this study presented a comprehensive understanding of the experience, and revealed the aspects which require interventions. However, one of the limitations of this study is that the participants were selected among elderly people using a single dementia care center. Therefore, the experience reported by participants may be different from the experience of PWED not using a dementia care center or those residing in nursing homes, so this should be taken into account in the interpretations of the results of this study.
Discussion
- This study explored the experience of accepting illness of PWED, including the essential elements of the experience, from a holistic perspective. The results of this study can be utilized as empirical data for the development of supportive interventions that can help PWED to incorporate their disease into their life and improve their quality of life. Based on the results of this study, the following suggestions are presented. First, it is necessary to conduct research to develop interventions for acceptance of illness of PWED, based on the constituents identified in this study. Second, the care of people with dementia is a long-term process in the context of the relationship between people with dementia and caregivers. Therefore, there is a need to conduct research on the experience of acceptance of illness in the context of care by recruiting people with dementia and their family caregivers together as participants so that they will pair up and participate together in research.
Conclusions
-
Conflict of interest
The author declared no conflict of interest.
-
Funding
None.
-
Authors’ contributions
Park, Jaewon contributed to conceptualization, data curation, formal analysis, methodology, visualization, writing-original draft, review & editing, investigation, and validation.
-
Data availability
Please contact the corresponding author for data availability.
NOTES
Acknowledgments
- 1. World Health Organization. A blueprint for dementia research [Internet]. Geneva: World Health Organization. 2022 [cited 2023 Mar 24]. Available from: https://www.who.int/publications/i/item/9789240058248
- 2. Parland PM, Kelly F, Innes A. Dichotomising dementia: Is there another way? Sociology of Health & Illness. 2017;39(2):258–269. https://doi.org/10.1111/1467-9566.12438Article
- 3. Global action plan on the public health responses to dementia 2017-2025 [Internet]. Geneva: World Health Organization. 2017 [cited 2023 Sep 24]. Available from: https://www.who.int/publications/i/item/global-action-plan-on-the-public-health-response-to-dementia-2017---2025
- 4. Kutzleben M, Schmid W, Halek M, Holle B, Bartholomeyczik S. Community-dwelling persons with dementia: What do they need? What do they demand? What do they do? A systematic review on the subjective experiences of persons with dementia. Aging & Mental Health. 2012;16(3):378–390. https://doi.org/10.1080/13607863.2011.614594Article
- 5. Read ST, Toye C, Wynaden D. Experiences and expectations of living with dementia: A qualitative study. Collegian. 2017;24(5):427–432. https://doi.org/10.1016/j.colegn.2016.09.003Article
- 6. Aldridge H, Fisher P, Laidlaw K. Experiences of shame for people with dementia: An interpretative phenomenological analysis. Dementia. 2019;18(5):1896–1911. https://doi.org/10.1177/1471301217732430ArticlePubMed
- 7. Biglan A, Hayes SC, Pistorello J. Acceptance and commitment: Implications for prevention science. Prevention Science : The Official Journal of the Society for Prevention Research. 2008;9(3):139–152. https://doi.org/10.1007/s11121-008-0099-4ArticlePubMedPMC
- 8. Hayes SC. Acceptance and commitment therapy, relational frame theory, and the third wave of behavioral and cognitive therapies – Republished article. Behavior Therapy. 2016;47(6):869–885. https://doi.org/10.1016/j.beth.2016.11.006ArticlePubMed
- 9. Zheng K, Bruzzese JM, Smaldone A. Illness acceptance in adolescents: A concept analysis. Nursing Forum. 2019;54(4):545–552. https://doi.org/10.1111/nuf.12368Article
- 10. Secinti E, Tometich DB, Johns SA, Mosher CE. The relationship between acceptance of cancer and distress: A meta-analytic review. Clinical Psychology Review. 2019;71:27–38. https://doi.org/10.1016/j.cpr.2019.05.001ArticlePMC
- 11. Cieślak K, Golusiński W. Coping with loss of ability vs. acceptance of disease in women after breast cancer treatment. Reports of Practical Oncology and Radiotherapy : Journal of Greatpoland Cancer Center in Poznan and Polish Society of Radiation Oncology. 2017;22(3):231–236. https://doi.org/10.1016/j.rpor.2017.01.001ArticlePMC
- 12. Obieglo M, Uchmanowicz I, Wleklik M, Jankowska-Polańska B, Kuśmierz M. The effect of acceptance of illness on the quality of life in patients with chronic heart failure. European Journal of Cardiovascular Nursing. 2016;15(4):241–247. https://doi.org/10.1177/1474515114564929ArticlePubMed
- 13. Lewko J, Polityńska B, Kochanowicz J, Zarzycki W, Okruszko A, Sierakowska M, et al. Quality of life and its relationship to the degree of illness acceptance in patients with diabetes and peripheral diabetic neuropathy. Advances in Medical Sciences. 2007;52(Suppl. 1):144–146. PubMed
- 14. Kurpas D, Mroczek B, Knap-Czechowska H, Bielska D, Nitsch-Osuch A, Kassolik K, et al. Quality of life and acceptance of illness among patients with chronic respiratory diseases. Respiratory Physiology & Neurobiology. 2013;187(1):114–117. https://doi.org/10.1016/j.resp.2013.02.009Article
- 15. Marthoenis M, Syukri M, Abdullah A, Tandi TMR, Putra N, Laura H, et al. Quality of life, depression, and anxiety of patients undergoing hemodialysis: Significant role of acceptance of the illness. The International Journal of Psychiatry in Medicine. 2021;56(1):40–50. https://doi.org/10.1177/0091217420913382ArticlePubMed
- 16. Holmner EP, Stålnacke BM, Enthoven P, Stenberg G. “The acceptance” of living with chronic pain – an ongoing process: A qualitative study of patient experiences of multimodal rehabilitation in primary care. Journal of Rehabilitation Medicine. 2018;50(1):73–79. https://doi.org/10.2340/16501977-2286Article
- 17. Silberfeld M, Rueda S. Krahn M, Naglie G. Content validity for dementia of three generic preference based health related quality of life instruments. Quality of Life Research. 2002;11:71–79. https://doi.org/10.1023/A:1014406429385ArticlePubMed
- 18. Woods RT. Discovering the person with alzheimer’s disease: Cognitive, emotional and behavioural aspects. Aging & Mental Health. 2001;5(Supplement 1):7–16. https://doi.org/10.1023/A:1014406429385Article
- 19. Aminzadeh F, Byszewski A, Molnar FJ, Eisner M. Emotional impact of dementia diagnosis: Exploring persons with dementia and caregivers’ perspectives. Aging & Mental Health. 2007;11(3):281–290. https://doi.org/10.1080/13607860600963695Article
- 20. Lyman KA. Bringing the social back in: A critique of the biomedicalization of dementia. The Gerontologist. 1989;29(5):597–605. https://doi.org/10.1093/geront/29.5.597ArticlePubMed
- 21. Lau WYT, Stoner C, Wong GHY, Spector A. New horizons in understanding the experience of Chinese people living with dementia: A positive psychology approach. Age and Ageing. 2021;50(5):1493–1498. https://doi.org/10.1093/ageing/afab097ArticlePubMed
- 22. Kitwood T. The experience of dementia. Aging & Mental Health. 1997;1(1):13–22. https://doi.org/10.1080/13607869757344Article
- 23. Kitwood T. Dementia reconsidered: The person comes first. Buckingham: Open university press; 1997. 160 p.Article
- 24. Wijngaarden E, Alma M, The AM. ‘The eyes of others’ are what really matters: The experience of living with dementia from an insider perspective. PLoS ONE. 2019;14(4):e0214724. https://doi.org/10.1371/journal.pone.0214724ArticlePubMedPMC
- 25. Górska SM, Maciver D, Forsyth K. Participation as means for adaptation in dementia: A conceptual model. Aging & Mental Health. 2021;25(3):499–511. https://doi.org/10.1080/13607863.2019.1695740Article
- 26. Tolhurst E, Weicht B. Preserving personhood: The strategies of men negotiating the experience of dementia. Journal of Aging Studies. 2017;40:29–35. https://doi.org/10.1016/j.jaging.2016.12.005ArticlePubMed
- 27. Lian Y, Xiao LD, Zeng F, Wu X, Wang Z, Ren H. The experiences of people with dementia and their caregivers in dementia diagnosis. Journal of Alzheimer's Disease : JAD. 2017;59(4):1203–1211. https://doi.org/10.3233/JAD-170370Article
- 28. Eriksen S, Helvik AS, Juvet LK, Skovdahl K, Førsund LH, Grov EK. The experience of relations in persons with dementia: A systematic meta-synthesis. Dementia and Geriatric Cognitive Disorders. 2016;42(5-6):342–368. https://doi.org/10.1159/000452404ArticlePubMed
- 29. Førsund LH, Grov EK, Helvik AS, Juvet LK, Skovdahl K, Eriksen S. The experience of lived space in persons with dementia: A systematic meta-synthesis. BMC Geriatrics. 2018;18(1):1–27. https://doi.org/10.1186/s12877-018-0728-0ArticlePubMedPMC
- 30. Eriksen S, Bartlett RL, Grov EK, Ibsen TL, Telenius EW, Rokstad AMM. The experience of lived time in people with dementia: A systematic meta-synthesis. Dementia and Geriatric Cognitive Disorders. 2021;49(5):435–455. https://doi.org/10.1159/000511225Article
- 31. Bjørkløf GH, Helvik AS, Ibsen TL, Telenius EW, Grov EK, Eriksen S. Balancing the struggle to live with dementia: A systematic meta-synthesis of coping. BMC Geriatrics. 2019;19(1):1–24. https://doi.org/10.1186/s12877-019-1306-9ArticlePubMedPMC
- 32. Poyser CA, Tickle A. Exploring the experience of the disclosure of a dementia diagnosis from a clinician, patient and carer perspective: A systematic review and meta-ethnographic synthesis. Aging & Mental Health. 2019;23(12):1605–1615. https://doi.org/10.1080/13607863.2018.1506747Article
- 33. Robinson L, Gemski A, Abley C, Bond J, Keady J, Campbell S, et al. The transition to dementia – individual and family experiences of receiving a diagnosis: A review. International Psychogeriatrics. 2011;23(7):1026–1043. https://doi.org/10.1017/S1041610210002437ArticlePubMed
- 34. Giorgi A. Phenomenology and psychological research. 16th ed. Pittsburgh: Duquesne University Press; 2012. 216 p.
- 35. Giorgi A. The descriptive phenomenological method in psychology: A modified Husserlian approach. 5th ed. Pittsburgh: Duquesne University Press; 2014. 233 p.
- 36. Giorgi A. The origins of the journal of phenomenological psychology and some difficulties in introducing phenomenology into scientific psychology. Journal of Phenomenological Psychology. 1998;29(2):161–176. https://doi.org/10.1163/156916298X00076Article
- 37. Lee NI. Phenomenology and qualitative research. Paju: Hangilsa; 2014. 419 p.
- 38. Giorgi A. The phenomenological movement and research in the human sciences. Nursing Science Quarterly. 2005;18(1):75–82. https://doi.org/10.1177/0894318404272112ArticlePubMed
- 39. Erlangsen A, Zarit SH, Conwell Y. Hospital-diagnosed dementia and suicide: A longitudinal study using prospective, nationwide register data. The American Journal of Geriatric Psychiatry. 2008;16(3):220–228. https://doi.org/10.1097/01.JGP.0000302930.75387.7eArticlePubMedPMC
- 40. Lincoln YS, Guba EG. Naturalistic Inquiry. Newbury Park: Sage Publications; 1985. 416 p.
- 41. Giorgi A. Phenomenology and the practice of science. Existential Analysis : Journal of the Society for Existential Analysis. 2010;21(1):3–22.
- 42. O'Rourke HM, Duggleby W, Fraser KD, Jerke L. Factors that affect quality of life from the perspective of people with dementia: A metasynthesis. Journal of the American Geriatrics Society. 2015;63(1):24–38. https://doi.org/10.1111/jgs.13178ArticlePubMed
- 43. Kyota A, Kanda K. How to come to terms with facing death: A qualitative study examining the experiences of patients with terminal cancer. BMC Palliative Care. 2019;18(1):1–10. https://doi.org/10.1186/s12904-019-0417-6ArticlePubMedPMC
References
Figure & Data
References
Citations


 KACHN
KACHN

 PubReader
PubReader ePub Link
ePub Link Cite
Cite