Articles
- Page Path
- HOME > Res Community Public Health Nurs > Volume 34(4); 2023 > Article
-
Original Article
- Factors Related to Smoking Relapse Within Six-Months of Smoking Cessation Among Inpatients
-
Ji Eun Bae1
 , Chul-Woung Kim2,3
, Chul-Woung Kim2,3 , Seung Eun Lee1
, Seung Eun Lee1 , Myungwha Jang4
, Myungwha Jang4
-
Research in Community and Public Health Nursing 2023;34(4):307-319.
DOI: https://doi.org/10.12799/rcphn.2023.00213
Published online: December 29, 2023
1Researcher, Daejeon·Sejong Tobacco Control Center, Center for Tobacco Control Research, Chungnam National University, Daejeon, Korea
2Director, Daejeon·Sejong Tobacco Control Center, Center for Tobacco Control Research, Chungnam National University, Daejeon, Korea
3Professor, Department of Preventive Medicine, College of Medicine, Chungnam National University, Daejeon, Korea
4Professor, Korea Human Resource Development Institute for Health and Welfare, Cheongju, Korea
- Corresponding author: Chul-Woung Kim 326, Department of Preventive Medicine, College of Medicine, Chungnam National University, 266, Munhwa-ro, Jung-gu, Daejeon, 35015, Korea Tel: +82-42-580-8268, Fax: +82-42-580-8395, E-mail: woung2@gmail.com
Copyright © 2023 Korean Academy of Community Health Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0) which allows readers to disseminate and reuse the article, as well as share and reuse the scientific material. It does not permit the creation of derivative works without specific permission.
- 1,317 Views
- 33 Download
Abstract
-
Purpose
- The purpose of this study is to identify factors associated with smoking relapse within 6 months after quit attempts among inpatients of a university hospital.
-
Methods
- The subjects of this study were 572 inpatients of the National University Hospitals in Daejeon & Sejong who had enrolled in the smoking cessation service provided by the Daejeon·Sejong Tobacco Control Center and attempted to quit smoking. The data used in the study were extracted from the Smoking Cessation Service Integrated Information System. The Kaplan-Meier method and Cox Proportional hazards model were used to identify variables associated with smoking relapse within 6 months.
-
Results
- The smoking relapse rate within 6 months was 76.7%, and variables associated with relapse included the absence of supporters for quitting smoking (hazard ratio [HR]=1.42, 95% confidence interval [CI]=1.00-2.02), nicotine dependence (HR=1.09, 95% CI=1.03-1.15), the use of prescription medications (including varenicline or bupropion) (HR=3.99, 95% CI=1.83-8.71), and the number of consultations (HR=0.67, 95% CI= 0.63-0.70).
-
Conclusion
- As a result of the study, the number of consultations showed the strongest correlation with abstinence within 6 months. This implies that it is necessary to increase the counseling participation rate of the subjects so that smoking cessation counseling can be continued after discharge, and it is also required to provide support education to guardians during hospitalization for effective smoking relapse prevention.
- Changes in health status such as disease diagnosis are an important factor that gives rise to a motivation for smoking cessation in smokers [1,2]. In particular, hospitalization due to disease gets smokers to pay more attention to their health, thereby make them more motivated to stop smoking, and causes them to more actively attempt to quit smoking. In addition, the hospital environment for inpatients is a favorable condition for smokers to attempt to quit smoking and maintain smoking cessation because inpatients have high accessibility to smoking cessation programs provided by the hospital, such as smoking cessation education, smoking cessation counseling, and pharmacotherapies, and all the spaces in a hospital are no smoking areas [3]. Actually, 51~60% of inpatients were reported to quit smoking voluntarily during hospitalization [4,5], and it was found that smoking cessation interventions provided for a short period of time led to the increased success rates of smoking cessation in patients [6,7]. Considering the effectiveness and efficiency of smoking cessation interventions, professional and systematic smoking cessation interventions for inpatients are believed to be necessary and important.
- Therefore, in an attempt to help inpatients to quit smoking, the Ministry of Health and Welfare implemented the inpatient smoking cessation support pilot program in 2016, and has implemented the inpatient smoking cessation program through 17 Regional Tobacco Control Centers since 2018 to ensure that inpatients can receive appropriate smoking cessation interventions. The 6-month smoking cessation success rate of the inpatient smoking cessation support pilot program was reported to be 55.8% [8], and this is about 3.7 times higher than the 6-month smoking cessation success rate of 15% after discharge in inpatients who quit smoking without receiving any interventions [9].
- However, smoking is a behavior with a high relapse risk, and a previous study reported that 78% of the people who attempted to quit smoking resumed smoking within 1 week from the quit date and 42% experienced smoking relapse within 6 months from the quit date [10]. It has been reported that the likelihood of smoking relapse decreases after maintaining smoking cessation for 6 months, and in this respect, the 6-month smoking abstinence rate can be viewed as a measure of long-term smoking cessation [11,12]. The purpose of smoking cessation is not quitting smoking for a short period of time but life-long smoking cessation, and the smoking cessation of inpatients influences the prognosis of underlying diseases, including the recurrence, mortality, and complications of diseases [8]. For these reasons, interventions for the prevention of smoking relapse are essentially required, but there have been relatively fewer studies of the smoking relapse of inpatients, compared to research on smoking relapse among general adult smokers [13-21]. In addition, a number of previous studies in Korea have the following limitations. First, in the majority of previous studies, the participants of each study were patients with a single disease such as acute myocardial infarction, cerebral infarction, and angina pectoris, so it is difficult to generalize study findings to all inpatients. Also, since most previous studies in Korea investigated the success or failure of smoking cessation over a relatively short period of 4~12 weeks, it is difficult to examine continuous abstinence rates over a period of 6 months or more. In addition, prior studies mainly conducted logistic regression analysis to identify factors associated with smoking relapse or smoking cessation success among inpatients. However, considering the results of Hughes et al. [11] that the participants showed variable patterns of smoking relapse over time after quitting smoking, it is necessary to investigate smoking relapse patterns by conducting a survival analysis because there is a need to examine the patterns of smoking relapse over a period from the starting point of smoking cessation to the time of smoking relapse and identify factors related to smoking relapse.
- Therefore, this study aimed to identify the patterns of smoking relapse over a period of 6 months from the quit date among people who used the inpatient smoking cessation program implemented by Daejeon·Sejong Tobacco Control Center(DTCC). Through this research, this study sought to present scientific bases required for the efficient operation of the inpatient smoking cessation program, and contribute to providing services that can help the inpatients to maintain smoking cessation.
Introduction
- 1. Study design
- This study is a retrospective survey study to identify factors affecting smoking relapse within 6 months from the date of the decision to quit smoking among the inpatients of two national university hospitals located in Daejeon and Sejong regions who received the inpatient smoking cessation service.
- The inpatient smoking cessation service is generally provided for 6 months from the date of enrollment in the inpatient smoking cessation program, and it is implemented by visiting the hospital room of the patient at least once a week during the hospital stay to deliver one-on-one personalized counseling services and additionally provide smoking cessation aids such as nicotine patches, gum, and lozenges if necessary. In addition, after providing education on pharmacotherapy for smoking cessation, it was checked whether the participant had intention to use prescription medicines for smoking cessation, and when the patient wanted to receive pharmacotherapy for smoking cessation, a request for collaborative treatment regarding pharmacotherapy was made to the department of family medicine in order to provide both pharmacotherapy and counseling for smoking cessation. When the patients who enrolled in the inpatient smoking cessation program were discharged from the hospital, face-to-face counseling was performed at 2, 4, 12, and 24 weeks from the date of the decision to quit smoking through the outpatient appointments of the hospital or through appointments for the visit to the DTCC, and telephone counseling was performed at 8, 16, and 20 weeks from the date of the decision to quit smoking. However, when a registrant was unable to participate in face-to-face counseling, it was replaced with telephone counseling.
- 2. Participants
- This study was conducted using the data of the users of the smoking cessation service program obtained from the smoking cessation integrated information system (nosmk.khealth.or.kr) of the Ministry of Health and Welfare and the Korea Health Promotion Institute. The participants were 732 persons who enrolled in the inpatient smoking cessation program provided by the DTCC from February, 2018 to July, 2021. The smoking cessation program started to be implemented in February, 2018, and the research data was obtained in July, 2021. Among the enrollees of the smoking cessation program, 572 persons who decided to quit smoking were finally selected as the participants of this study by excluding 160 persons who did not have intention to quit smoking.
- Regarding the inclusion criteria, the participants were selected from people who had the intention to quit smoking among the inpatients admitted to all the wards of national university hospitals located in Daejeon and Sejong regions. To screen the inpatients for the intention to quit smoking, when patients were hospitalized, the ward nurses initially examined the current smoking status of patients when they filled out the nursing information form of the electronic medical record (EMR), and the nurses asked the patients identified as smokers to apply for smoking cessation counseling if they wanted to. Afterwards, when a request for smoking cessation counseling was submitted to the DTCC, a smoking cessation counselor from the center visited the patient’s room in the hospital, and explained the smoking cessation support service to the patient. Then, after confirming the patient’s intention to quit smoking, the screening process for registering the patient was carried out. During the screening process, patients who did not wish to receive the smoking cessation support service, patients who were not able to communicate due to reasons such as a comatose state, and patients who were using other public smoking cessation support services such as the smoking cessation clinics of public health centers were excluded from the selection of participants.
- 3. Measures
- The sociodemographic characteristics examined in this study were as follows: gender, age, education level, social security regarding health coverage, alcohol intake in the past year, and regular exercise in the past year. Education level was classified into middle school or below, high school, and junior college/university or higher. Social security regarding health coverage was categorized into national health insurance and medical aid, and ‘Do not know’ or no response (including refusal to respond) was treated as a missing value. Drinking status or alcohol intake in the past year refers to whether the respondent consumed alcohol in the past year regardless of the type of alcohol. The performance of regular exercise in the past year was assessed by examining whether the patient performed moderate-intensity physical activities (physical activities that cause a person to feel slightly out of breath more than normal or make the heart rate slightly higher than normal) for 10 minutes or more at least once a week in the past year.
- This study analyzed the following smoking-related characteristics: the presence of a supporter for quitting smoking, the presence of previous quit attempts, the age of smoking initiation, the period of smoking (pack-years) and nicotine dependence. The presence of supporters for quitting smoking refers to the presence or absence of people who helped the person to quit smoking, including family members, colleagues at work, and healthcare professionals. Regarding the presence of previous quit attempts, it was examined whether the participant had ever attempted to quit smoking in the past year. For the age of smoking initiation, the participants were asked to write their age or the year when they smoked cigarettes for the first time. Regarding the period of smoking (pack years), one pack year was defined as smoking a pack of cigarettes a day for one year, and the total pack year was calculated by multiplying the average smoking amount per day (pack) by the total period of smoking (years). The level of nicotine dependence was measured using a Korean Version of the Fagerström Test for Nicotine Dependence (K-FTND). FTND was developed by Heatherton et al. [22], and it is the most commonly used method to measure nicotine dependence. It consists of a total of 6 items, and the total scores range from 0 to 10. A total score is calculated by summing the scores of all six questions, and higher total scores indicate higher levels of nicotine dependence, and a total score of 7 points or more is classified as a high level of dependence on nicotine. K-FTND was created by Ahn et al. [23] by translating the original version of FTND. This tool has been shown to have satisfactory levels of reliability and validity, so it has been used in many studies as a measure of nicotine dependence in Korean smokers [7,12]. The value of Cronbach’s α was reported as .61 in Heatherton et al. [22] and as .69 in Ahn et al. [23]. It was calculated as .61 in this study.
- Attitude toward smoking cessation was assessed by measuring the following three subdomains of attitude as variables: importance of quitting smoking, confidence in quitting smoking, and readiness in quitting smoking [12,24]. Each subdomain of attitude was measured with a single question on a 10-point Likert scale. In other words, respondents were asked to select a response within the range of 0 to 10 points, and higher scores indicated higher levels of importance of quitting smoking, confidence in quitting smoking, and readiness in quitting smoking. The levels of importance of quitting smoking, confidence in quitting smoking, and readiness in quitting smoking were respectively measured using the following questions: How important is quitting smoking to you?; (2) How confident are you that you will succeed in quitting smoking?; (3) How much are you ready to quit smoking?
- This study examined the following characteristics related to smoking cessation interventions: the number of counseling sessions, the use of pharmacotherapeutic smoking cessation aids (nicotine replacement therapies, NRTs) such as nicotine patches, gum, and lozenges, and the use of prescription medicines for smoking cessation (varenicline and bupropion). The frequency of counseling is the total number of counseling sessions including both face-to-face and telephone consultations provided from the date of enrollment in the inpatient smoking cessation program to the completion time of the consultations, and it was used as a continuous variable in the analysis. The use of pharmacotherapeutic smoking cessation aids (NRTs) or prescription medicines for smoking cessation (bupropion and varenicline) was dichotomously categorized into ‘Use’ and ‘No use.’ In other words, it was classified as ‘Use’ when the participant used NRTs or prescription medicines for smoking cessation at least once during the period of the smoking cessation service program, and it was classified as ‘No use’ when the participant had never used them during the period.
- In this study, the dependent variable was smoking relapse status. Smoking relapse means resuming smoking after a period of abstinence. In this study, it refers to resuming smoking within 6 months after deciding to quit smoking through enrollment in an inpatient smoking cessation program. Smoking relapse was assessed by examining whether the person maintained smoking cessation through self-reports. At this time, smoking relapse was defined as ‘smoking 3 or more cigarettes within 6 months after starting an attempt to quit smoking’ according to the criterion of the guidelines of the regional smoking cessation private subsidy program [25].
- In this study, the duration of smoking abstinence was used as the time variable to analyze factors associated with smoking relapse within 6 months after enrollment in the inpatient smoking cessation program. The duration of smoking abstinence was defined as the period from the date of the decision to quit smoking to the date of the final evaluation and confirmation of continued smoking abstinence, and it was calculated in days.
- 4. Data collection and analysis
- This study received approval for the data use from the Ministry of Health and Welfare and the Korea Health Promotion Institute through the application procedure for the use of project results (Research Management No. 2021-023), and this research was conducted after obtaining approval from the Institutional Review Board of Chungnam National University (IRB No. 202106-SB-114-01).
- Regarding the research data, the items of the registration form (registration card) and the counseling record form (counseling card) of the inpatient smoking cessation program were utilized as the major variables of this study, and these data were obtained from the integrated smoking cessation service information system (nosmk.khealth.or.kr). The information of the registration form was acquired through a face-to-face interview with each patient when the patient registered for the inpatient smoking cessation program, and the patients themselves were asked to complete the form based on their current status at the time of registration during the interview. The content of the counseling record form was written based on the counselor’s consultations with individual participants in a face-to-face manner or over the phone during the service period
- The collected data was analyzed using SPSS 24.0 to examine differences in the characteristics of participants between people who resumed smoking within 6 months and those who continuously abstained from smoking for 6 months, examine the patterns of smoking relapse according to the duration of smoking abstinence, and identify factors associated with smoking relapse within 6 months. First, a univariate analysis was performed using the t-test and χ2-test to comparatively analyze the differences between the characteristics of participants between smoking relapsers and abstinent smokers, and a survival curve was generated using the Kaplan-Meier method to examine the patterns of smoking relapse according to the duration of smoking abstinence.
- Next, a multivariate analysis was conducted using the Cox proportional hazard model to identify factors affecting smoking relapse within 6 months after enrollment in the inpatient smoking cessation program. The time variable was set as the duration of abstinence, and the event variable was set as smoking relapse within 6 months after enrollment in in the inpatient smoking cessation program. As a result of the assessment of the multicollinearity of the explanatory variables used in Cox regression analysis, the tolerance values of all variables were greater than 0.1 and the variance inflation factor (VIF) was 1.04-2.16, indicating that there was no problem of multicollinearity.
Methods
1) Sociodemographic characteristics
2) Smoking-related characteristics
3) Attitude toward smoking cessation
4) Characteristics related to smoking cessation interventions
5) Smoking relapse status and the duration of smoking abstinence
- 1. Comparison of characteristics of smoking relapsers and abstinent smokers over a 6-month period
- This study was conducted with a total of 572 participants, and their sociodemographic characteristics were as follows (Table 1). In gender, males accounted for 94.2% (539 people) and females took up 5.8% (33 people). The mean age was 54.47 years. For education level, high school (33.4%, 191 people) accounted for the largest proportion, followed by college/university or higher (32.2%, 184 people), and middle school or below (14.9%, 85 people). Regarding the type of social security regarding healthcare coverage, 78.7% (450 people) were enrolled in national health insurance and 6.6% (38 people) were medical aid beneficiaries. With respect to smoking-related characteristics, 86.7% (496 people) had a supporter for smoking cessation, and 31.8% (182 people) reported having previously attempted to quit smoking. The average age of smoking initiation was 20.34 years, and the average period of smoking was 34.24 pack-years. The mean score for nicotine dependence was 4.39 points. In terms of characteristics related to smoking cessation interventions, 16.6% (95 people) used smoking cessation aids (NRTs), and 2.3% (13 people) used prescription medicines for smoking cessation (varenicline, bupropion). However, there was no significant difference in sociodemographic characteristics, smoking-related characteristics, and the use of NRTs or prescription medications among characteristics related to smoking cessation interventions between the group who resumed smoking within 6 months (the relapser group) and the group who had been continuously abstinent from smoking throughout 6 months (the abstainer group).
- As a result of the comparison of characteristics of participants between the relapser group who relapsed to smoking within 6 months and the abstainer group who continuously abstained from smoking for 6 months, there was a significant difference in the levels of importance of quitting smoking, confidence in quitting smoking, and readiness in quitting smoking, which are the subdomains of attitude toward smoking cessation. Also, there was a significant difference in the frequency of counseling among the characteristics related to smoking cessation interventions. More specifically, scores for importance of quitting smoking (p=.049), readiness in quitting smoking (p=.005), and confidence in quitting smoking (p<.001) were lower in the relapser group (8.29 points, 7.09 points, and 7.54 points) than in the abstainer group (8.68 points. 7.98 points, and 8.21 points). The frequency of counseling was lower in the relapser group (4.80 session) than the abstainer group (9.25 sessions) (p<.001).
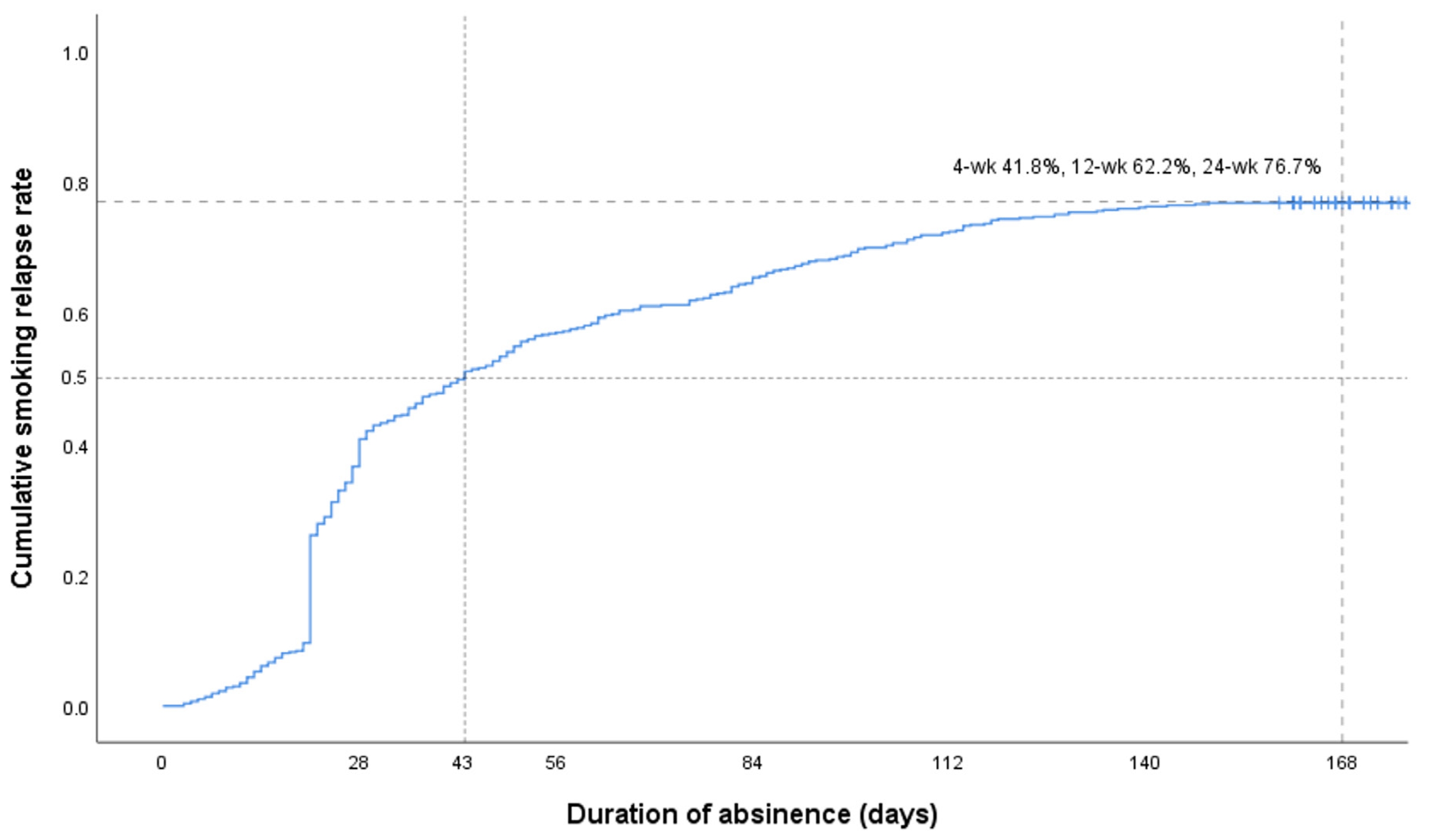
- 2. The pattern of smoking relapse according to the duration of smoking abstinence
- Among the 572 participants who registered for the inpatient smoking cessation program and decided to quit smoking, the smoking relapse rate within 6 months was 76.7% (439 people), and the smoking cessation maintenance rate was 23.3% (133 people). The average survival period from the date of the decision to quit smoking to the time of smoking relapse was 109.68 days, and the survival period when 50% of the participants survived or continuously abstained from smoking was 43.00 days. Regarding the time of smoking relapse, among the participants who failed to continuously abstain from smoking, the group who resumed smoking within 4 weeks from the date when they decided to quit smoking constituted the largest proportion 41.8% (239 people), and the survival curve for the cumulative smoking relapse rate shows a sharp increase in the slope of the curve until 4 weeks after the decision to quit smoking (Figure 1). As shown in Figure 1, the cumulative smoking relapse rates over a period after 4 weeks showed the pattern of a relatively gradual increase. More specifically, 20.4% (117 people) resumed smoking within 4 weeks to 12 weeks, and 14.5% (83 people) resumed smoking over a period within 12 weeks to 6 months (Table 2).
- 3. Factors associated with smoking relapse within 6 months
- The variables that showed a significant association with smoking relapse within 6 months among people who decided to quit smoking were identified as the presence of a supporter for smoking cessation, nicotine dependence, the frequency of counseling, and the use of prescription medicines for smoking cessation (p<.05). The use of NRTs was also identified as a significant variable, but this variable was significant by a narrow margin (p=.050) (Table 3). Specifically, the risk for smoking relapse was 1.42 times higher in the group without a supporter for smoking cessation than the group with at least one supporter for smoking cessation (hazard ratio(HR)=1.42, 95% confidential interval(CI)=1.00~2.02, p=.049). Also, it was found that as the score for nicotine dependence was increased by one point, the risk for smoking relapse was increased by 1.09 times (HR=1.09, 95% CI=1.03~1.15, p=.002). In terms of smoking cessation intervention variables, as the frequency of counseling was increased by one session, the risk for smoking relapse was decreased by 33% (HR=0.67, 95% CI=0.63~0.70, p<.001). On the other hand, the risk for smoking relapse was 3.99 times higher in the group who used prescription medicines for smoking cessation than the group who did not use them (HR=3.99, 95% CI=1.83~8.71, p=.001).
Results
- The majority of prior studies on the smoking cessation of inpatients in Korea provided participants with smoking cessation programs developed by hospitals themselves, and mainly analyzed factors related to the achievement of continued smoking abstinence within 4 to 12 weeks [13-21]. This study is differentiated from such previous studies in that it investigated the smoking relapse rate within 6 months from the date of the decision to quit smoking and factors related to smoking relapse among the patients who enrolled and participated in the inpatient smoking cessation program that is a government-supported community service program implemented by Regional Tobacco Control Centers.
- The comparison of the characteristics of participants between the group who resumed smoking within 6 months (the relapser group) and the abstainer group who continuously abstained from smoking for 6 months (the abstainer group) revealed that there were significant differences in the attitude toward smoking cessation (importance of quitting smoking, confidence in quitting smoking, and readiness to quit smoking) and the frequency of counseling between the two groups. The levels of importance of quitting smoking, confidence in quitting smoking, and readiness to quit smoking, which indicate the assessments of attitudes toward quitting smoking, can be regarded as indicators that represent the motivation levels for smoking cessation among the participants. In this study, scores for importance of quitting smoking, confidence in quitting smoking, and readiness in quitting smoking were higher in the abstainer group than the relapser group, and these results indicated that the abstainer group was more motivated to quit smoking. Meanwhile, the mean score for attitudes toward smoking cessation was 7.09 points or higher in both groups. In particular, the mean score for importance of quitting smoking was 8.29 points or higher. In previous studies conducted with general adult populations and adolescents, the mean score for importance of quitting smoking was reported as 6.73~8.12 points, and the mean score for confidence in quitting smoking, as 5.64 to 7.06 points, and the mean score for readiness in quitting smoking as 5.41 to 7.51 points [26-28]. Compared to these results of previous studies, the mean scores for attitudes toward smoking cessation were relatively higher in this study. These results are thought to indicate that as inpatients recognized the need to quit smoking as a result of increased interest in health due to the occurrence of the disease, they showed a high level of motivation to quit smoking. Regarding the frequency of counseling, the average number of counseling sessions in the relapse group was 4.80 sessions, which was significantly lower than 9.25 sessions in the abstinence group. This finding is consistent with the results of a study by Shin et al. [19], which showed that the number of counseling sessions was lower in the group who failed to quit smoking than the group who succeeded in smoking cessation.
- In the present study, among the patients using the inpatient smoking cessation program, the smoking relapse rate within 6 months was 76.7%, and this means that 23.3% of the participants continuously abstained from smoking for 6 months. The smoking relapse rate in this study was a little higher compared to the 6-month smoking relapse rate of 68% reported in a previous study of inpatients by Shin et al. [19]. However, in a study by Shin et al., the residents and nurses of the department of family medicine provided 6-month-long one-on-one smoking cessation counseling to patients referred to the smoking cessation clinic of the department of family medicine within the hospital, and 32.1% of the participants actively used prescription medicines for smoking cessation such as varenicline or bupropion. On the other hand, in this study, the smoking cessation counseling service were provided by counselors from the DTCC, who were not the medical staff of the hospital, and only 2.3% of the participants were prescribed medicines for smoking cessation. In this regard, it has been reported that provision of smoking cessation advice and education by professional medical staff had a significantly greater effect on smoking cessation [6,29]. In addition, the use of prescription medications such as varenicline in combination with counseling has been shown to be more effective for prolonged smoking abstinence [30-32]. Thus, it is thought that these differences in smoking cessation intervention methods contributed to the above-mentioned difference in the smoking relapse rate between this study and a previous study [19]. With respect to foreign studies conducted not with inpatients but with the general population, a previous study reported that when only smoking cessation counseling was provided, the 6-month continuous abstinence rates of smokers were about 10-12% [33], and other previous studies revealed that when both pharmacotherapy for smoking cessation and smoking cessation counseling were provided, the continuous abstinence rates of smokers were about 20-30% [12,34]. In this study, the 6-month continuous abstinence rate among inpatients was a similar level to the results of previous studies.
- Factors related to smoking relapse within 6 months among inpatients were the presence of the supporter for quitting smoking, nicotine dependence, the frequency of counseling, and the use of prescription medicines for smoking cessation. In particular, smoking cessation intervention characteristics, such as the frequency of counseling and the use of prescription drugs for smoking cessation, were found to have a strong association with the risk for smoking relapse.
- Although social support for smoking cessation is theoretically considered an important factor in maintaining smoking cessation [35], some previous clinical trial studies reported inconsistent and contradictory findings [20,36-38]. The results of this study indicated that the presence of supporters for quitting smoking positively influenced the prevention of smoking relapse among inpatients who decided to quit smoking. These results are consistent with a prior study of smoker patients who used the smoking cessation clinics of public hospitals [20]. The study reported that the continuous abstinence rate was higher in the group who lived with one or more family members than the group who did not [20]. Similarly, a previous study of male workers from small and medium-sized enterprises also found that the likelihood of smoking cessation success for 6 months was 1.9 times higher in the group with a supporter for quitting smoking such as the spouse or other family members than in the group without any supporters for quitting smoking [38]. Meanwhile, it has been reported that the significant influence of supporters for quitting smoking on the maintenance of smoking cessation is also related to the support behavior of supporters for smoking cessation [36,39-40]. In particular, a previous study reported that the positive behaviors of supporters for smoking cessation positively influenced the maintenance of smoking cessation, but negative behaviors such as criticism about smoking may lead to smoking relapse [36]. These results suggest that in order to reduce the smoking relapse rate in inpatients, it is necessary to implement systematic education for supporters for smoking cessation so that guardians can perform their role as supporters for quitting smoking in a positive direction.
- Nicotine dependence indicates the degree of addiction to the nicotine component contained in cigarettes. It is generally known that a higher level of nicotine dependence is associated with more severe withdrawal symptoms when an attempt to quit smoking are made, and thus it is linked to a greater likelihood of failure to quit smoking [41]. The results of this study also showed that a higher level of nicotine dependence was associated with a higher risk for smoking relapse, and these results are consistent with the findings of a previous study of the users of the smoking cessation clinic of public health centers, which reported that a lower level of nicotine dependence was linked to a higher smoking cessation success rate [42].
- Regarding the characteristics related to smoking cessation interventions, the examination of the relationship between the frequency of counseling (the number of counseling sessions) and the risk for smoking relapse showed that a higher frequency of counseling was associated with a lower smoking relapse rate. As a general rule, the inpatient smoking cessation program normally provides at least one session of 30-minute individual counseling during hospitalization, and continuously offers one-on-one face-to-face counseling or phone counseling for six months after discharge, thereby delivering a total of 9 sessions of counseling after discharge. A number of previous studies have reported that the number of smoking cessation counseling sessions is closely related to the maintenance of smoking cessation [27-28,41,43-45]. Miller et al. [29] also reported that the 1-year continuous abstinence rate was higher in the group that received counseling for 3 months after discharge, compared to the general counseling group that received the physician’s recommendation to quit smoking during hospitalization. In a study of patients referred to the smoking cessation clinic of a general hospital, Shin et al. [19] also reported that a higher number of counseling sessions for smoking cessation after discharge was associated with a higher smoking cessation success rate. These study findings suggest that the provision of continuous smoking cessation counseling after discharge as well as smoking cessation counseling during hospitalization has a strong association with the prevention of smoking relapse and the maintenance of smoking cessation.
- Regarding the use of prescription drugs for smoking cessation among the characteristics related to smoking cessation interventions, the risk for smoking relapse was four times higher in the group who used prescription medicines for smoking cessation than in the group who did not use them. This result is in contrast to the previous findings that both varenicline and bupropion, which are prescription drugs for smoking cessation, increased the rate of long-term smoking cessation attempts, and in particular, varenicline was more effective for smoking cessation than NRT products [30-32,46]. In this study, out of 572 participants, only 13 people used smoking cessation drugs, so caution is needed in interpreting the research results, and further research is required to accumulate more research results in the future.
- This study has the following limitations. First, smoking relapse status, the dependent variable of this study, was examined through self-reports, which represent subjective assessments. Although it is necessary to assess smoking relapse through physiological indicators such as the measurement of exhaled carbon monoxide concentration and a urine cotinine test, the assessment method was limited to self-reports in this study. This is due to the fact that the self-report method was realistically more suitable and feasible because only 11.1 to 50.8% of the participants visited the hospital for outpatient treatment and participated in the physiological measurement when the assessment of the maintenance of abstinence from smoking was performed at 4 weeks, 12 weeks, and 24 weeks. In the future, follow-up research should be conducted on an objectively measured dependent variable by increasing the physiological measurement rate. Second, this study used the data from the integrated smoking cessation service information system of the Korea Health Promotion Institute. Since this study analyzed only the standardized data of the results of the national smoking cessation support service program presented by the institute, variables related to the characteristics related to hospitalization, such as the main diseases of participants, were not reflected in the study results. As a result, this study did not provide sufficient discussion on smoking relapse in relation to variables related to hospitalization. Therefore, in the future studies, there is a need to analyze characteristics related to hospital admission by including them as variables and using a more sophisticated research design. Third, the value of Cronbach alpha of K-FTND used to measure nicotine dependence in this study was .61, and this is the same value as the value of Cronbach alpha reported by the creator of FTND [22]. It is thought that since the instrument contains only 6 items, the level of reliability was calculated as a relatively low value [22]. However, considering that FTND is the most commonly used instrument that provides a measure of the nicotine dependence of smokers in Korea as well as in other countries, there is a need to conduct an in-depth analysis of the reliability of the nicotine dependence assessment tool in the future.
- Despite the above-mentioned limitations of this research, it is considered meaningful that this study examined smoking abstinence rates over a period of 6 months and analyzed factors related to smoking relapse among all the inpatients of two university hospitals who had intent to quit smoking.
Discussion
- This study applied the Cox proportional hazards model to identify factors associated with smoking relapse over time within 6 months from the date of the decision to quit smoking among the inpatients of university hospitals who used the inpatient smoking cessation program of the DTCC.
- The results of this study revealed that a lower risk for smoking relapse was associated with the presence of supporters for smoking cessation, a lower level of nicotine dependence, and a higher number of counseling sessions. These results showed that personalized smoking cessation counseling considering the characteristics of the participants of the inpatient smoking cessation program had a positive effect on the prevention of smoking relapse and the maintenance of smoking cessation among the participants of the smoking cessation program. Since the number of counseling sessions is an important factor for continuous smoking abstinence, it is important to increase the rate of participation in counseling even after hospital discharge by paying attention to the formation of rapport between the patients receiving counseling and the counsellor during hospitalization. Additionally, there is a need to develop a system for smoking cessation counseling linked to the outpatient treatment schedule after discharge, and it is also necessary to secure a stable location for smoking cessation counseling. Further, in order to support the smoking abstinence behavior of hospitalized smokers, it is necessary to provide support for the guardians of smoker patients by providing appropriate education materials as well as systematic education programs for supporters for smoking cessation to ensure that the guardians of patients can perform the role of positive supporters for smoking cessation not only during hospitalization but also after discharge.
- Based on the study findings described above, it is suggested that further research should be conducted on factors related to smoking cessation success among inpatients according to characteristics related to hospitalization, based on the rates of smoking abstinence verified by biomarkers. In addition, it is necessary to conduct research on the development and effectiveness of education programs for supporters for quitting smoking among the guardians of inpatients.
Conclusions
-
Conflict of interest
The authors declared no conflict of interest.
-
Funding
This study was supported by Health Promotion Fund, Ministry of Health&Welfare, Republic of Korea(2021-023) and Chungnam National University academic research fund.
-
Authors’ contributions
Bae, Ji Eun contributed to conceptualization, data curation, formal analysis, methodology, project administration, visualization, and writing-original draft, review & editing. Kim, Chul-Woung contributed to conceptualization, funding acquisition, methodology, project administration, writing – original draft, review & editing, and supervision. Lee, Seung Eun contributed to conceptualization, methodology, project administration, and writing – original draft, review & editing. Jang, Myungwha contributed to conceptualization, methodology, and writing – review & editing.
-
Data availability
Please contact the corresponding author for data availability.
NOTES
Acknowledgments
- 1. Fagerström KO. Measuring degree of physical dependence to tobacco smoking with reference to individualization of treatment. Addictive Behaviors. 1978;3(3-4):235–241. https://doi.org/10.1016/0306-4603(78)90024-2ArticlePubMed
- 2. Copeland AL, Brandon TH. Testing the causal role of expectancies in smoking motivation and behavior. Addictive Behaviors. 2000;25(3):445–449. https://doi.org/10.1016/S0306-4603(99)00003-9ArticlePubMed
- 3. Park EW, Cheong YS. Physicians’ perspectives on the smoking cessation service for inpatient smokers. Korean Journal of Health Promotion. 2019;19(3):128–137. http://doi.org/10.15384/kjhp.2019.19.3.128Article
- 4. Glasgow RE, Stevens VJ, Vogt TM, Mullooly JP, Lichtenstein E. Changes in smoking associated with hospitalization: Quit rates, predictive variables, and intervention implications. American Journal of Health Promotion. 1991;6(1):24–29. https://doi.org/10.4278/0890-1171-6.1.24ArticlePubMed
- 5. Noonan D, Karvonen-Gutierrez CA, Duffy SA. Differences in risk perception, and quit rates among hospitalized veteran pipe smokers, cigarette smokers and dual users. Journal of Addictions Nursing. 2014;25(2):89–93. https://doi.org/10.1097/JAN.0000000000000028ArticlePubMedPMC
- 6. Seon WS, Yeo JK, Baek SH, Koh YS, Cho HJ. Physician’s recommendations for smoking cessation to patients with smoking-related diseases. Journal of the Korean Academy of Family Medicine. 1996;17(12):1423–1429.
- 7. Murray RL, Leonardi-Bee J, Marsh J, Jayes L, Li J, Parrott S, Britton J. Systematic identification and treatment of smokers by hospital based cessation practitioners in a secondary care setting: cluster randomized controlled trial. BMJ. 2013;347:f4004. http://doi.org/10.1136/bmj.f4004ArticlePubMedPMC
- 8. Jung YS. Development of a smoking cessation service for inpatient smokers. Seoul: Korea Health Promotion Institute; 2017. 264 p.
- 9. Duffy SA, Scholten RL, Karvonen-Gutierrez CA. The relation of tobacco use during hospitalization to post-discharge smoking cessation among US veterans. Preventive Medicine. 2010;50(5-6):285–287. https://doi.org/10.1016/j.ypmed.2010.01.012ArticlePubMed
- 10. Herd N, Borland R, Hyland A. Predictors of smoking relapse by duration of abstinence: Findings from the International Tobacco Control (ITC) four country survey. Addiction. 2009;104(12):2088–2099. https://doi.org/10.1111/j.1360-0443.2009.02732.xArticlePubMedPMC
- 11. Hughes JR, Peters EN, Naud S. Relapse to smoking after 1 year of abstinence: A meta-analysis. Addictive Behaviors. 2008;33(12):1516–1520. https://doi.org/10.1016/j.addbeh.2008.05.012ArticlePubMedPMC
- 12. Lee SE, Kim CW, Im HB, Jang MW. Patterns and predictors of smoking relapse among inpatient smoking intervention participants: A 1-year follow-up study in Korea. Epidemiology and Health. 2021;43:e2021043. https://doi.org/10.4178/epih.e2021043ArticlePubMedPMC
- 13. Jun WH, Yun HS. Effects of smoking cessation education for patients with percutaneous coronary intervention. Korean Journal of Adult Nursing. 2012;24(3):274–283. http://doi.org/10.7475/kjan.2012.24.2.274Article
- 14. Kong JH, Hai Y. Effects of a smoking cessation program including telephone counseling and text messaging using stages of change for outpatients after a myocardial infarction. Journal of Korean Academy of Nursing. 2013;43(4):557–567. http://doi.org/10.4040/jkan.2013.43.4.557ArticlePubMed
- 15. Kim ES, Choi HO. Effects of a smoking cession program using telephone counselling and text messaging for patients after ischemic heart disease. Journal of the Korea Academia-Industrial Cooperation Society. 2014;15(12):7248–7258. http://doi.org/10.5762/KAIS.2014.15.12.7248Article
- 16. Cho SH. Effects of a smoking cessation education on smoking cessation, endothelial function, and serum carboxyhemoglobin in male patients with variant angina. Journal of Korean Academy of Nursing. 2012;42(2):190–198. http://doi.org/10.4040/jkan.2012.42.2.190ArticlePubMed
- 17. Jung KY, Yoo SH, Ma SH, Hong SH, Lee YS, Shim UY, et al. Inpatient smoking cessation program and its success rate for abstinence among Korean smokers. Korean Journal of Family Medicine. 2009;30(7):503–510. https://doi.org/10.4082/kjfm.2009.30.7.503Article
- 18. Lee YH, Oh GJ, Han MH, Kim GJ, Park HY, Kim HS, et al. The effect of a hospital-based smoking cessation intervention on the continuous abstinence rate from smoking over 12 months in patients with cerebral infarction. Korean Journal of Health Education and Promotion. 2016;33(3):61–70. http://doi.org/10.14367/kjhep.2016.33.3.61Article
- 19. Shin HY, Lee YJ, Kim SH, Cho HJ. Factors associated with six month quit rate of in-hospital smoking program. Journal of the Korean Society for Research on Nicotine and Tobacco. 2016;7(2):66–73. https://doi.org/10.25055/JKSRNT.2016.7.2.66Article
- 20. Hwang EJ. Related factors of smoking cessation success and maintenance of patients using smoking cessation clinic at a public hospital: Focused on patient demographics and smoking related factors. Journal of the Korea Academia-Industrial Cooperation Society. 2019;20(3):535–543. https://doi.org/10.5762/KAIS.2019.20.3.535Article
- 21. Lee YH, Han MH, Lee MR, Jeong JW, Kim NH, Oh SK, et al. Continuous abstinence rate from smoking over 12 months according to the frequency of participation in a hospital-based smoking cessation program among patients discharged after acute myocardial infarction. Korean Journal of Health Promotion. 2016;16(1):48–55. https://doi.org/10.15384/kjhp.2016.16.1.48Article
- 22. Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The fagerström test for nicotine dependence: A revision of the fagerström tolerance questionnaire. British Journal of Addiction. 1991;86(9):1119–1127. https://doi.org/10.1111/j.1360-0443.1991.tb01879.xArticlePubMed
- 23. Ahn HK, Lee HJ, Jung DS, Lee SY, Kim SW, Kang JH. The reliability and validity of Korean version of questionnaire for nicotine dependence. Korean Journal of Family Medicine. 2002;23(8):999–1008.
- 24. Boudreaux ED, Sullivan A, Abar B, Bernstein SL, Ginde AA, Camargo Jr CA. Motivation rulers for smoking cessation: A prospective observational examination of construct and predictive validity. Addiction Science & Clinical Practice. 2012;7(1):1–9. https://doi.org/10.1186/1940-0640-7-8ArticlePubMedPMC
- 25. Ministry of Health and Welfare, Korea Health Promotion Institute. A guide to regional tobacco control centers in 2018. Guideline. Sejong: Ministry of Health and Welfare; 2018 November. Report No: 11-1352000-000901-10.
- 26. Kim JS, Kang SJ, Kim DJ, Choi IN, Choi BS. Success factors of new enrollees at smoking cessation clinics in the nationwide public health centers in Korea based on gender differences. Korean Public Health Research. 2018;44(1):17–30. http://doi.org/10.22900/kphr.2018.44.1.002Article
- 27. Jin BJ, Kim CW, Lee SE, Im HB, Lee TY. Factors related to smoking recurrence within six-months smoking cessation among employees in enterprises with smaller than 300 workers. Research in Community and Public Health Nursing. 2021;32(1):107–115. https://doi.org/10.12799/jkachn.2021.32.1.107Article
- 28. Bae JE, Kim CW, Lee SE, Im HB, Kim IY, Lee TY, et al. Factors related to the smoking relapse of out-of-school adolescents. Korean Journal of Health Education and Promotion. 2021;38(3):13–21. https://doi.org/10.14367/kjhep.2021.38.3.13Article
- 29. Miller NH, Smith PM, DeBusk RF, Sobel DS, Taylor CB. Smoking cessation in hospitalized patients: Results of a randomized trial. Archives of Internal Medicine. 1997;157(4):409–415. https://doi.org/10.1001/archinte.1997.00440250059007ArticlePubMed
- 30. Chang CP, Huang WS, You CH, Hwang LC, Lu IJ, Chan HL. Factors correlated with smoking cessation success in older adults: A retrospective cohort study in Taiwan. International Journal of Environmental Research and Public Health. 2019;16(18):3462. https://doi.org/10.3390/ijerph16183462ArticlePubMedPMC
- 31. Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: An overview and network meta-analysis. Cochrane Database of Systematic Reviews. 2013;(5):CD009329. https://doi.org/10.1002/14651858.CD009329.pub2ArticlePubMed
- 32. Anthenelli RM, Benowitz NL, West R, Aubin LS, McRae T, Lawrence D, et al. Neuropsychiatric safety and efficacy of varenicline, bupropion, and nicotine patch in smokers with and without psychiatric disorders (EAGLES): A double-blind, randomised, placebo-controlled clinical trial. The Lancet. 2016;387(10037):2507–2520. https://doi.org/10.1016/S0140-6736(16)30272-0ArticlePubMed
- 33. Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database of Systematic Reviews. 2017;3(3):CD001292. https://doi.org/10.1002/14651858.CD001292.pub3ArticlePubMedPMC
- 34. Nohlert E, Öhrvik J, Tegelberg Å, Tillgren P, Helgason ÁR. Long-term follow-up of a high- and a low-intensity smoking cessation intervention in a dental setting- a randomized trial. BMC Public Health. 2013;13(1):592. https://doi.org/10.1186/1471-2458-13-592ArticlePubMedPMC
- 35. Westmaas JL, Bontemps-Jones J, Bauer JE. Social support in smoking cessation: Reconciling theory and evidence. Nicotine & Tobacco Research. 2010;12(7):695–707. https://doi.org/10.1093/ntr/ntq077ArticlePubMed
- 36. Park IH. Effect of enhancing partner support to improve smoking cessation: a meta-analysis. Journal of the Korean Academy of Family Medicine. 2002;23(3):301–312.
- 37. Babalola F, Kimber PR, Scheuermann TS, Park EW. Enhancing partner support to improve smoking cessation. Cochrane Database of Systematic Reviews. 2018;8(8):CD002928. https://doi.org/10.1002/14651858.cd002928.pub4ArticlePubMedPMC
- 38. Ryu IH, Park KS. Successful factors of smoking cessation for male workers from small and medium enterprises registered with local tobacco control center. Journal of Agricultural Medicine and Community Health. 2021;46(4):253–265. https://doi.org/10.5393/JAMCH.2021.46.4.253Article
- 39. Roski J, Schmid LA, Lando HA. Long-term associations of helpful and harmful spousal behaviors with smoking cessation. Addictive Behaviors. 1996;21(2):173–185. https://doi.org/10.1016/0306-4603(95)00047-XArticlePubMed
- 40. Park EH. Effect of spousal support on smoking cssation outcome of self-quitters. Journal of the Korean Academy of Family Medicine. 2006;27(8):652–658.
- 41. Lee KJ, Chang CJ, Kim MS, Lee MH, Cho YH. Factors associated with success of smoking cessation during 6 months. Journal of Korean Academy of Nursing. 2006;36(5):742–750. https://doi.org/10.4040/jkan.2006.36.5.742ArticlePubMed
- 42. Kim CH, Seo HG. The factors associated with success of smoking cessation at smoking-cessation clinic. Journal of the Korean Academy of Family Medicine. 2001;22(11):1603–1611.
- 43. Kim MJ, Jeong IS. Smoking relapse and related factors within one year among successes of the smoking cessation clinics of public health centers. Journal of Preventive Medicine and Public Health. 2011;44(2):84–92. https://doi.org/10.3961/jpmph.2011.44.2.84ArticlePubMed
- 44. Kim YS, Kim YH. The patterns and risk factors of smoking relapse among people successful in smoking cessation at the smoking cessation clinics of public health centers. Research in Community and Public Health Nursing. 2011;22(4):365–376. https://doi.org/10.12799/jkachn.2011.22.4.365Article
- 45. Lee GH, Lee KM, Jung SP. A comparison of the factor analysis on smoking cessation success between inpatient smoking cessation program and residential smoking cessation program. Korean Journal of Health Promotion. 2021;21(3):83–91. https://doi.org/10.15384/kjhp.2021.21.3.83Article
- 46. Stead LF, Koilpillai P, Fanshawe TR, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2016;3(3):CD008286. https://doi.org/10.1002/14651858.CD008286.pub2ArticlePubMed
References
Figure & Data
References
Citations


 KACHN
KACHN

 PubReader
PubReader ePub Link
ePub Link Cite
Cite