Articles
- Page Path
- HOME > Res Community Public Health Nurs > Volume 34(2); 2023 > Article
-
Review Article
- Factors Related to Diabetes Self-Care among Immigrants in the United States: A Scoping Review
-
Jung Eun Kim

-
Research in Community and Public Health Nursing 2023;34(2):171-182.
DOI: https://doi.org/10.12799/rcphn.2023.00094
Published online: June 30, 2023
Assistant Professor, Mennonite College of Nursing, Illinois State University, US
- Corresponding author: Kim, Jung Eun Illinois State University, Mennonite College of Nursing, Campus Box 5810 Normal, IL 61790 Tel: 1-309-438-7400, E-mail: jkim133@ilstu.edu
Copyright © 2023 Korean Academy of Community Health Nursing
This is an Open Access article distributed under the terms of the Creative Commons Attribution NoDerivs License. (http://creativecommons.org/licenses/by-nd/4.0) which allows readers to disseminate and reuse the article, as well as share and reuse the scientific material. It does not permit the creation of derivative works without specific permission.
- 938 Views
- 58 Download
Abstract
-
Purpose
- The purpose of this scoping review was to explore related factors in diabetes self-care among immigrants in the U.S. Diabetes is one of the fastest-growing chronic illnesses, but little is known about factors in self-care among minority immigrants in the U.S.
-
Methods
- The Arksey and O’Malley (2005) methodological framework guided this review, which examined 16 articles, including qualitative, quantitative, and mixed-methods designs. PRISMA guidelines were used with five Databases. Search terms included: immigrants in the U.S., type 2 diabetes, self-care, and self-management.
-
Results
- Factors related to diabetes self-care among immigrants were identified: (1) changed dietary lifestyle, (2) low economic and health insurance, (3) social support and resources, (4) low English proficiency, (5) psychological contexts, and (6) gender roles.
-
Conclusion
- Given the culturally unique related factors in diabetes self-care among immigrants, healthcare professionals must be knowledgeable and responsive to the ethnic minority immigrants’ needs to promote effective diabetes self-care.
- Diabetes is one of the chronic diseases with the quickest rate of increase in the 21st century. The number of people with diabetes has tripled in the past two decades [1]. Type 2 diabetes (T2D) is the most prevalent form of diabetes, accounting for about 90% of cases. As of 2021, approximately 537 million adults (20-79 years) worldwide were living with diabetes [1]. By 2045, this number will reach 700 million. Immigrants from racial and ethnic minorities are disproportionately affected by diabetes in the U.S. (US) [2]. American Indians and Alaska Natives, black or African Americans, Latinos or Hispanics, Asian Americans, Native Hawaiians, and other Pacific Islanders are among these racial and ethnic minority immigrants. Immigrants from ethnic minorities have a higher prevalence [3] and burden [4] of managing diabetes than whites, as well as more complications [3]. According to a number of studies, obstacles for ethnic immigrants in the U.S. include language barriers, a lack of health professional awareness of cultural health preferences, and a lack of culturally adapted interventions [5]. Despite advances in medical technology and expanding access to health care, ethnic minority immigrants continue to face disadvantages in maintaining optimal health due to these obstacles.
- Diabetes necessitates ongoing self-care or self-management in order to prevent further complications and deterioration [6]. Ineffective self-care for T2D can result in acute and long-term complications (such as skin and eye complications, neuropathy, and functional disability) and even death [6]. Self-care for diabetes is however complex and challenging, involving multiple tasks such as medication regimen, diet control, blood sugar monitoring, and routine medical visits [7]. Self-care for diabetes requires patients to make substantial lifestyle adjustments. Cultural differences among ethnic minority immigrants may influence their diabetes self-care, health care decision-making, and relationships with health care providers [8]. Identifying and understanding the context that facilitates and affects diabetes self-care would strengthen future interventions and education that are culturally tailored. However, few studies have examined and investigated the associated factors, facilitators, challenges, and barriers in diabetes self-care among ethnic immigrants in the US. This scoping review aimed to examine factors related to T2D self-care among immigrants in the US.
Introduction
- This scoping review utilized five stages based on Arksey and O'Malley's [9] guidelines to examine T2D self-care related factors among ethnic minority immigrants in the US. This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [10,11]. The stages are listed below.
- Stage 1: Identifying the Research Questions and Eligibility Criteria
- The research objective was to explore factors related to diabetes self-care among immigrants in the US. The research questions were as follows:
- 1. What sample and settings were included in each study?
- 2. What were the diabetes self-care related factors among immigrants in the U.S.?
- 3. How different were the diabetes self-care related-factors, challenges and barriers among different ethnic immigrants?
- The article selection criteria were as follows: (1) aimed at adult immigrants with diabetes; (2) centered on self-care or self-management of T2D; (3) conducted in the U.S.; (4) published between 2010 and 2021; (5) peer-reviewed studies; and (6) published as an academic journal in English.
- Exclusion criteria were as follows: (1) included childhood group in the participants, (2) included other chronic illnesses, and (3) conducted in other countries, not in the U.S..
- Stage 2: Identifying Relevant Publications
- Five databases were consulted for this review: CINAHL, Health Source Nursing Academic Edition, Medline Plus, PsycInfo, and Sociology Index (SOCIndex). We searched these databases for articles published between 2010 and 2021.
- Stage 3: Selecting Publications
- The search included three constructs (i.e., immigrants in the U.S., self-care, and diabetes). The following search combinations were used: (“immigrants in the U.S.”) AND (“self-care” OR “self-management”) AND (“diabetes type 2” OR “diabetes mellitus type 2” OR “diabetes 2”). The search included qualitative, quantitative studies, and published reviews in English reporting on self-care among immigrants with diabetes in the U.S.
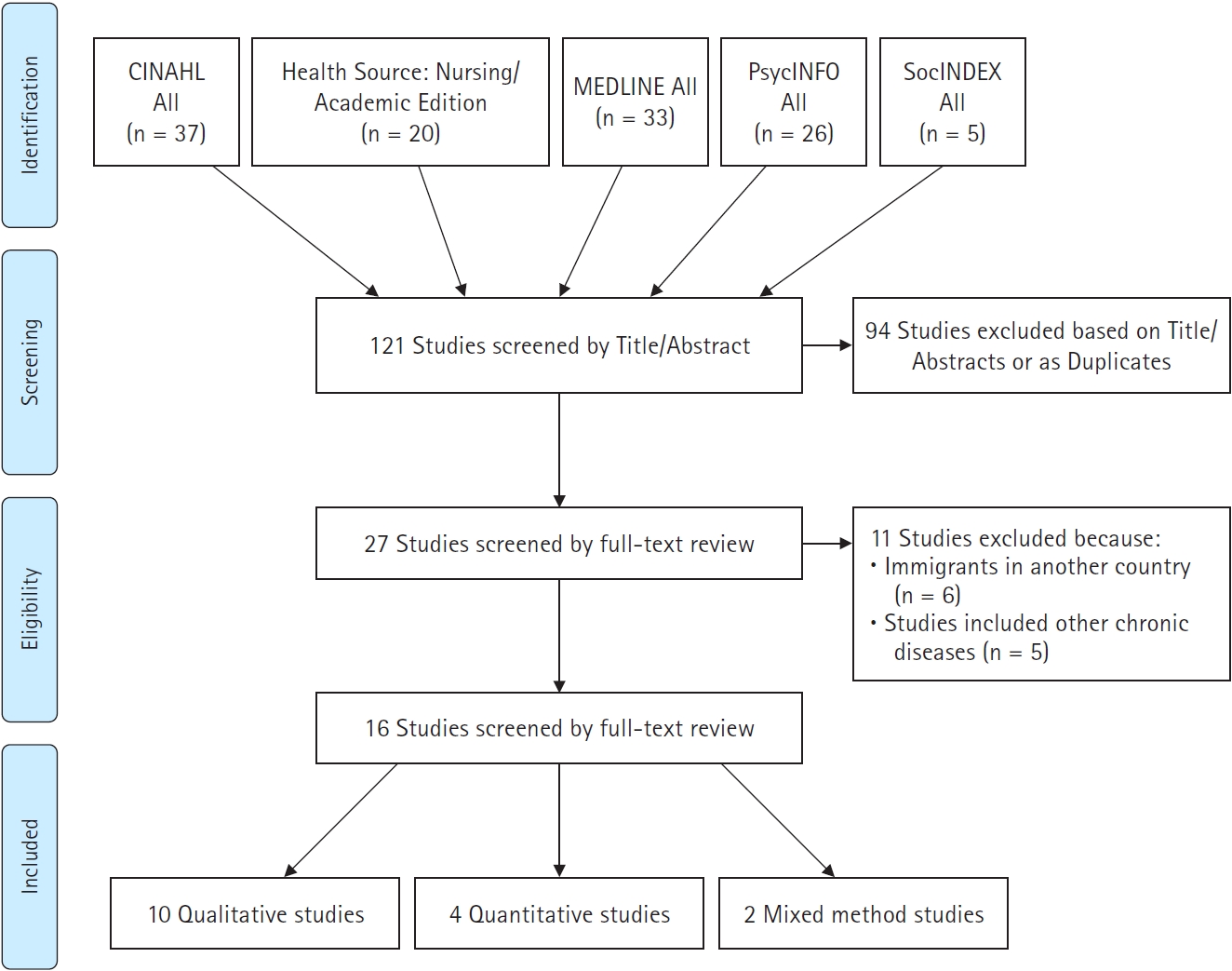
- Stage 4: Charting the Data (PRISMA Figure 1)
- 121 articles were retrieved by applying the inclusion and exclusion criteria and utilizing the major key terms. From the 121 articles, 94 were eliminated due to their title, abstract, or duplication. A thorough full-text review of the remaining 27 articles was conducted, and 16 articles meeting the eligibility criteria were selected (Figure 1).
- Stage 5: Collating, Summarizing, and Reporting the Results
- The articles included in this scoping review are listed in Table 1. Ethnic immigrants from China, South Korea, Mexico, Sub-Saharan Africa, Haiti, Somalia, Middle Eastern countries (Iran, Turkey, and Lebanon), and Latin American countries participated in the selected studies. Ten articles employed qualitative methods, four employed quantitative methods, and two employed mixed methods.
Methods
- Study Characteristics
- Among the 16 articles, four articles focused on Chinese immigrants [12-15]. The other four articles were about Korean immigrants [16-19], and three focused on Hispanic immigrants [20-22]. The other four articles included Sub-Saharan African [23], Haitian immigrants [24], Middle-Eastern immigrants [25], and Somali immigrants [26]. Last one article focused on East Asian immigrants from four Asian countries, including China, Japan, South Korea, and Taiwan [27]. The participants’ age range in the 16 selected articles was from 27 to 86. The mean number of participants in 10 qualitative studies and four qualitative studies was approximately 28 and 206, respectively. All participants in the 16 articles reported that they had been diagnosed with T2D for at least one year and were self-identified immigrants.
- After data analysis, six major themes were identified as factors related to T2D self-care among immigrants in the U.S.: changed dietary lifestyle, low economic status and health insurance, social support and resources, low English proficiency, psychological contexts, and gender roles.
- Changed Dietary Lifestyle
- For managing diabetes, dietary modification presented a significant obstacle for ethnic immigrants. According to six studies [12-17,20,23,25], when immigrants attempted to change their eating habits and dietary lifestyle, they encountered obstacles. The participants in Cha's [16] study reported having difficulty adhering to diabetic dietary recommendations. Maintaining traditional Korean views of food, a lack of culturally sensitive diabetic diet guidelines, and locating American foods that satisfied their taste preferences in the United States were the obstacles. Traditional Korean "good" foods include meat, poultry, and white steamed rice. Vegetables and multigrain rice (e.g., barley rice) are considered "bad" or "poor" foods among Koreans, particularly among older Koreans. Koreans believe that sick individuals should consume "good" food to restore their health, regardless of the quantity of "good" food consumed. These beliefs inhibit the diabetic immigrants from Korea from adopting a diabetic diet and lifestyle. The recommended diabetic diet affects the spouses of diabetic Korean immigrants. In the study by Choi [17], spouses of Korean immigrants with diabetes most frequently mentioned a diabetic diet. For instance, the husband of a female Korean immigrant with diabetes stated that he was a terrible husband because he ate his preferred white rice at every meal with his wife. Even though he was aware that his wife liked white rice and had trouble adhering to a diabetic diet, he ate his preferred Korean foods. The husband felt guilty because he did not consume the same foods as his wife.
- According to Chesla [12], the Chinese immigrants' diet posed the greatest difficulty in managing their diabetes. Rice has many cultural and historical connotations for the Chinese, including the maintenance of holistic health and well-being [12]. Therefore, replacing white rice with "tasteless" brown, red, or black rice is a difficult task. According to Chesla [12], the restriction of rice could cause emotional distress and depression. Diabetic diets complicate social interactions such as family outings, meals, and celebrations.
- In regards to dietary restrictions, family members feel obligated to the patients, but they also recognize the value of social comfort and enjoyment. Therefore, some immigrants are hesitant to disclose their diabetes to their friends and are distressed when the topic is brought up at social gatherings. Additionally, McConatha and colleagues [25] reported that dietary modification was a source of stress. For immigrants from the Middle East, family gatherings involve sharing large, traditional meals. The ceremonial meals and family gatherings are a source of family pride and heritage because they serve as a symbolic link to their homelands. However, their traditional dishes typically contain a great deal of carbohydrates.
- In addition, if a guest does not consume a substantial amount of food, it may reflect negatively on the host's hospitality. When Kindarara and colleagues investigated the experiences of Sub-Saharan African immigrants with diabetes self-care, the majority of participants reported dietary difficulties [23]. These immigrants struggled to adjust to not eating rice and consuming fewer of their traditional foods. One participant noted that not eating favorite foods, not craving high-carbohydrate foods, and adopting a diabetic diet were obstacles; they noted that in their culture, they do not feel satisfied if they do not eat rice. They felt loss when staple native foods were reduced or eliminated. Across these diverse cultures, dietary modification was identified as a significant diabetes management challenge. According to several participants in Hu's [20] study, adjusting their own methods of food preparation and consumption was the most difficult diabetes-related obstacle.
- Low Economic Status and Health Insurance
- In the U.S., immigrant T2D self-care is influenced by their low socioeconomic status and lack of health insurance [14,16,18,23,26]. The research conducted by Chun and colleagues revealed that immigrant participants had to deal with economic hardships and poverty in the United States, which increased their acculturative stress [14]. By limiting their access to health care services, the financial hardship had a direct and negative impact on their ability to self-manage their diabetes. One participant in the study reported feeling "caught between two worlds." They were not eligible for government health care subsidies and could not afford comprehensive health insurance. They felt socially excluded and anxious about their diabetes treatment and overall health. In a study by Njeru [26], Latino respondents reported that the cost of managing T2D was a significant barrier. The elderly participants of Joo's [18] study reported having financial difficulties due to the high cost of diabetes care. The majority of study participants were retired and lived on fixed incomes. Despite receiving social security benefits and assistance from their children, they felt overwhelmed by diabetes-related costs. Kindarara and colleagues also found that a lack of health insurance and a low income made it more difficult for patients to obtain medical care or adhere to diabetic diet recommendations [23].
- Due to their low socioeconomic status, immigrants with diabetes must work long hours and may not have time for self-care. They consume readily available foods such as fast food [23]. Their low socioeconomic status makes it difficult for them to adhere to diabetic dietary recommendations and practice optimal self-care. According to Cha [16], the majority of Koreans who immigrate to the U.S. are relatively young and healthy, so they may not need health insurance. However, when they are diagnosed with chronic diseases such as diabetes, it is likely that they will not qualify for health insurance coverage due to the nature of their employment (e.g., small business, temporary job) or because they have a low income or a preexisting health condition. Uninsured or underinsured Korean immigrants with diabetes did not have access to the majority of new oral advanced medications or insulin. More participants with poorly controlled diabetes than those with controlled diabetes reported insurance difficulties.
- Social Support and Resources
- In relation to self-care among immigrants, social support and resources were discussed as factors with diverse perspectives [15-18,20,23,25].
- Cha and colleagues found that young adult Korean immigrants, many of whom ran small family businesses, lacked time for diabetes self-care [16] due to their long work hours. Their primary source of social support was limited to Sunday church activities, and they reported difficulty adhering to diabetes recommendations. Older Korean immigrants relied on free or low-cost community resources in the United States, including ethnic senior daycare centers, the YMCA, Medicare and/or Medicaid programs.
- Choi and colleagues examined the role of spouse support in diabetes self-care among older Korean immigrants [17]. Some spouse participants stated that their role was to encourage and assist, but that the patient was ultimately responsible for his or her own care. In contrast, other spouse participants stated that it was their duty to learn more about diabetes, assist with self-management, and provide ongoing support. Participants with diabetes and their spouses identified spousal support and recognizing diabetes self-care as a team effort as essential components of successful self-management. The results of a study conducted by Chun and colleagues revealed that participants with greater social support had lower HbA1c levels and lower levels of depression [15].
- In a study of Hispanic immigrants, Hu and colleagues identified a lack of support from health care providers and family members as a significant barrier to diabetes management [20]. Participants compared their diabetes management to navigating in the dark. Participants felt helpless due to their perception that health care providers paid little attention to their disease. Participants required assistance and support from their families, but dietary issues led to family conflicts. Although family members wanted to help, they lacked the knowledge necessary to assist participants with diabetes. Due to the necessary changes in lifestyle, such as diet and exercise, patients with diabetes are unable to effectively manage self-care without family support. In addition, Hispanic immigrants with diabetes reported a lack of financial resources for disease management due to the absence of support from health care providers and families.
- Kindarara and colleagues identified four subcategories of social support in diabetes self-care among immigrants from Sub-Saharan Africa [23]: (1) family and peer support, (2) provider-patient relationship, (3) spirituality, and (4) resources for T2D self-care. Family and peer support were the most frequently mentioned source of emotional support among the four subcategories of social support. Children, parents, and especially spouses provided medication reminders, monitoring, encouragement, transportation to medical appointments, and meal preparation assistance. The participants in Kindarara's [23] study also regarded the healthcare provider-patient relationship and the relationship with God as significant sources of emotional support.
- According to McConatha and colleagues, despite the importance of social support for effective coping, social support is reciprocally affected by the changes patients must make to manage their illnesses [25]. About 90% of participants in McConatha's [25] study reported that changes in diet and exercise habits negatively affected their relationships with family and friends, especially during social gatherings. In addition, the participants stated that their families and friends provided them with hope and strength. Social and emotional support from family and friends was cited as the most influential factor in their ability to successfully alter their lifestyles.
- Low English Proficiency
- Low English proficiency was one of the immigrant diabetes self-care barriers [8, 14, 18]. Low English proficiency was a crucial acculturation stressor that limited healthcare access for Chinese immigrants with diabetes, according to Chun and colleagues [14]. Low English proficiency hindered not only communication with health care providers, but also the ability to perform daily self-care tasks, such as scheduling medical appointments and purchasing over-the-counter health products (e.g., glucose monitor patches). These diabetes self-care requirements became a source of stress and anxiety. Their sense of self-efficacy in managing diabetes and general health was diminished by language barriers. According to the research conducted by Nam [19] and Joo [18], Korean immigrants viewed the language barrier and limited access to health care services as significant obstacles to managing diabetes. The majority of Korean immigrants do not speak English, limiting their access to adequate health care services. Many Korean immigrants are unsure of the progression of their illness and are unable to participate in educational sessions due to their limited English proficiency. Even though they want to ask physicians questions, they struggle to read and comprehend information about T2D self-management.
- Inadequate English proficiency restricts their access to health care services and causes discomfort in daily life. The limited access to health care services among elderly Korean immigrants with diabetes is also attributed to their lack of diabetes knowledge, which is a result of their limited English proficiency. One of the participants in Nam's [19] study reported that her mother died from a low blood sugar level. Her mother's limited English proficiency resulted in inadequate knowledge of her illness. She believed that she should avoid eating sweets to prevent high blood sugar, so she did not eat them. However, one day, she suddenly fainted and died on the way to the emergency room. Some may argue that this story is unique to elderly Korean immigrants. Nonetheless, it is evident that limited language proficiency is one of the most significant barriers to diabetes management among immigrants who did not grow up in the U.S.
- Psychological Contexts: Depression, Loneliness, Social Isolation, and Unstable Emotion
- Four studies [12,14,20,25] discussed psychological issues in diabetes self-care among immigrants, including depression, loneliness, social isolation, and emotional instability. In Chesla's [12] study, Chinese immigrants expressed concern about diabetic dietary restrictions. When they attempted to strictly adhere to the diabetic diet, they experienced depression and emotional imbalance. The participants also stated that life would be meaningless without delicious food. Remarkably, the Chinese immigrants had trouble adhering to the diabetic diet in Chinese restaurants, which caused them to withdraw from social interactions during meals. This circumstance impacts their social interactions, which are fundamental to their emotional health. Chesla [12] discovered that Chinese immigrants with uncontrolled glucose levels exhibited increased irritability and emotional instability, such as temper tantrums. Their irritability had a negative impact on family harmony, but their spouses felt obligated to forgive their outbursts as part of their care.
- Similarly, Chinese participants in Chun's [14] study reported increased feelings of isolation, loneliness, and depression in relation to diabetes self-care. These psychological issues vary by ethnic and cultural background. For instance, in Chun's [14] study, some participants reported distinct acculturation experiences regarding filial piety and respect for the elderly since moving to the United States. Traditionally, the majority of sons and daughters in China take care of their elderly parents. However, since moving to the United States, their adult children have adopted western cultural values and weakened family ties and responsibilities. The more elderly Chinese parents fear losing family support from their adult children, while the elderly Chinese experience emotional distress and resignation regarding their unloyal offspring.
- In McConatha's [25] study, all Middle Eastern immigrants reported stress and anxiety related to diabetes self-management. Their daily lives are affected by their anxiety and stress. Additionally, 90% of the participants experienced loss of personal identity and loneliness. One older participant in McConatha's [25] study reported that meal-centered social gatherings became less enjoyable and even stressful. The immigrants with diabetes were required to limit their social activities, particularly those involving alcohol and food. They perceived that their friends and family treated them differently, as if they were more fragile, which marginalized and isolated them socially. In the study conducted by Hu [20], Hispanic immigrants with diabetes also described emotional suffering such as depression, isolation from family, a sense of hopelessness, and a sense of being different in their self-care. Particularly when they experience complications associated with diabetes, such as diabetic retinopathy, they feel hopeless and despondent [20].
- Gender Roles
- According to the findings of two studies [19,20], female immigrants were more susceptible to diabetes management difficulties than male immigrants. Traditionally, Korean women are responsible for preparing family meals and staying at home [19]. After immigration to the United States, both men and women work long hours. As a result, many diabetic Korean immigrant women struggle to maintain their traditional roles while working hard outside the home. If a man has diabetes, he is more likely to receive assistance from his spouse in managing diabetes; however, if a woman has diabetes, she is more likely to continue preparing regular meals for her family rather than maintaining a diabetic diet for herself. Compared to Korean male immigrants, Korean female immigrants with diabetes face gender-related obstacles in effectively managing their condition. In addition, Hu [20] found that female participants with diabetes had difficulty preparing different foods for themselves compared to the food preferences of their family members. The family members of the female participants were not accustomed to a diabetic diet, so to avoid conflict, the female participants gave up their dietary restrictions.
- McConatha [25] also demonstrated that female immigrants with diabetes have more difficulty altering their diet than male immigrants. The majority of male participants reported not being responsible for cooking; they relied on their spouses to successfully manage their diet. Despite the fact that female participants were better cooks than their male counterparts, they reported greater difficulty making the necessary dietary changes for diabetic self-care. According to Cha [16], when diabetic women prepare meals based on ADA recommendations, their families are unsatisfied. Therefore, the women with diabetes experience tension and conflict between their previous family diet and their new diabetes diet. Ultimately, the women with diabetes make sacrifices for their families and adhere to family-approved recipes.
- According to Chun [14], male immigrants with diabetes experienced a loss of gender roles as a result of their condition. Due to diabetes-related dietary restrictions, he ate less rice, thereby diminishing his physical strength. Due to diminished physical strength, he was unable to actively fulfill his role as a provider for the household and faced gender role reversals.
Results
- Self-care is essential for people with chronic illnesses such as T2D. However, self-care is complicated. Ineffective diabetes self-care may cause acute or long-term effects, including skin and eye complications, neuropathy, functional disability, hypertension, stroke, and death risk [6].
- T2D self-care for immigrants in the U.S. is associated with their cultures and traditions. Williams [29] characterized ethnicity as "a complex multidimensional construct reflecting the convergence of biological factors, geographical origins, culture, political, economic, and legal factors." Depending on their ethnicity and culture, different approaches are required to comprehend disparities in health and health care [30]. The findings of this scoping review highlight the need for future research that investigates the factors associated with effective self-care among immigrants with diabetes in the U.S.
- Dietary changes posed particular difficulties, as was a recurring theme in the reviewed articles. Dietary changes can negatively impact social gatherings and relationships with family and friends for immigrants. Due to the symbolic ties to their homelands, these traditional foods are associated with cultural pride and heritage and are shared with family and friends. Diet-related cultural conflicts influence the self-care practices of immigrants with diabetes. Additional research and health care providers are required to identify the food culture of ethnic groups and develop a diabetic diet that is culturally appropriate.
- Regarding low economic status and lack of health insurance, racial and ethnic immigrants have historically been plagued by health disparities resulting from an unfair distribution of resources such as health care, education, and politics [31]. Higher morbidity and mortality rates indicate that the health of underrepresented minority groups in the U.S. has remained inferior to that of white Americans [32]. Undoubtedly, the high rates of un-insurance among ethnic minority groups indicate health disparities. Most immigrants received their education in their home countries. Therefore, they must exert more effort to work and earn a living in the U.S. than their native American counterparts. To establish themselves in a new country, the majority of them must endure hardship. Due to these barriers to immigration, their precarious economic situation and lack of health insurance make it more difficult for them to maintain optimal health. In order to have a more equitable health service system, the U.S. has been reforming its health legislation, but it still does not meet the requirements of minority immigrants. Particularly, undocumented immigrants are more vulnerable in terms of Medicaid eligibility and receiving insurance premium credits [33]. For minority immigrants to receive optimal healthcare services, healthcare providers and political legislators must collaborate.
- Social support served as a predictor, a mediator, and occasionally an impediment to T2D self-care activities. The most prevalent source of social support was family and friends. In addition to family and friends, there were also churches, healthcare providers, and community-based services. However, depending on ethnicity, age, and culture, social support and resources played various roles. Most immigrants indicated that family, friends, and churches help them manage their diabetes. On the other hand, some immigrants reported conflicts with family members and friends when performing self-care activities. Their lifestyle changes affect their family and friends’ life as well. Suppose family and friends are not knowledgeable about diabetes or do not understand its characteristics. In that case, they may have a bias against the person with diabetes, which could lead to dinnertime conflicts. Nevertheless, despite these conflicts, it is undeniable that lack of social support is identified as a significant barrier to diabetes self-care among immigrants [20,25]. Particularly, Asian culture emphasizes family unity more than individual needs [34]. Older Asian immigrants rely on the assistance of their adult children rather than seeking professional health care services.
- This scoping review revealed that language inadequacy was one of the most important determinants of T2D self-care. Low English proficiency impeded not only communication with healthcare providers but also the acquisition of the skills necessary to perform daily self-care tasks independently. Previous works have demonstrated that language and cultural differences are obstacles when seeking adequate health care [35]. Older ethnic immigrants are likelier to have lower English proficiency than younger ones. Due to the higher prevalence of chronic disease among elderly immigrants, language translation services are more crucial for their access to health care.
- Diverse factors were associated with the psychological contexts of ethnic immigrants with diabetes who practiced self-care. Changes in cultural norms, lifestyles, socioeconomic status, and language barriers all contribute to the stressful nature of immigration to a new culture. If the immigrants are elderly and arrived in the U.S. at a later age, they must face additional barriers and obstacles when performing diabetes self-care activities. They experienced anxiety, cultural disconnection, loneliness, and social isolation while attempting diabetes self-care. The psychological contexts of diabetes self-care may differ based on age, gender, socioeconomic status, and family and friend relationships. Health care providers should continue to be concerned about the psychological context-related vulnerability of immigrants with diabetes and develop effective strategies for them.
- An intriguing finding of this review was the gender roles in self-care among immigrants with diabetes in the U.S. Female immigrants with diabetes typically have more difficulty maintaining traditional gender roles than their male counterparts. As mothers or wives, many immigrant women with diabetes serve their families' preferred meals rather than diabetic diet foods. Female immigrants were more susceptible to engaging in activities of self-care. Depending on the ethnic culture and family culture, however, the gender role can be discussed from various angles. Additional research is required to identify gender roles among immigrants with diabetes and to comprehend the effects of gender roles on diabetes self-care.
- Limitations
- Despite the thoroughness of this scoping review, this scoping review may have overlooked some relevant studies. Additional relevant studies may be searched using more specific search terms and other databases. While most studies employ qualitative methods, the findings cannot be generalized due to small samples.
- This scoping review includes quantitative, qualitative, and mixed method studies. In consequence, this review lacks statistical evidence and synthesized results. There also may be a need for more consistency among the included studies as a result of combining diverse method studies into one. Moreover, there is no assessment of methodological quality or risk of bias in included studies. However, despite these limitations, this scoping review addresses broader questions and provides valuable evidence by adhering to well-defined methodological guidelines and reporting standards.
- Implications
- Immigrants of various racial and ethnic backgrounds living in the U.S. are identified as having diabetes. The discussions indicate the need for additional research on the health and diabetes self-care of immigrants of diverse ethnic backgrounds. In the future, researchers who share the ethnic, cultural, and linguistic perspectives of study participants are required to conduct additional research on ethnic culture sensitivity and uniqueness.
Discussion
- This scoping review described research findings pertaining to culturally specific factors in diabetes self-care among immigrants in the U.S. The review suggests that related self-care factors among ethnic immigrants with diabetes must be examined in light of their unique culture, and that health care providers should develop culturally appropriate care plans. It is the responsibility of health care professionals to assess, acknowledge, and respect a patient's culture and to consider their characteristics in order to promote optimal health.
Conclusion
-
Conflict of interest
The authors declared no conflict of interest.
-
Funding
None.
-
Authors’ contributions
Kim, Jung Eun contributed to conceptualization, formal analysis, methodology, project administration, visualization, and writing - original draft, review & editing.
-
Data availability
Not applicable.
NOTES
Acknowledgments
- 1. International Diabetes Federation.org [Internet]. Brussels: Diabetes facts and figures; [cited 2023 Mar 15]. Available from: https://idf.org/about-diabetes/facts-figures/
- 2. Chow EA, Foster H, Gonzalez V, McIver L. The disparate impact of diabetes on racial/ethnic minority populations. Clinical Diabetes. 2012;30(3):130–133. https://doi.org/10.2337/diaclin.30.3.130Article
- 3. Golden SH, Brown A, Cauley JA, Chin MH, Gary-Webb TL, Kim C, et al. Health disparities in endocrine disorders: Biological, clinical, and nonclinical factors--An endocrine society scientific statement. The Journal of Clinical Endocrinology and Metabolism. 2012;97(9):E1579–1639. https://doi.org/10.1210/jc.2012-2043ArticlePubMedPMC
- 4. Centers for Disease Control and Prevention.gov [Internet]. Atlanta: National diabetes statistics report; [cited 2023 Mar 15]. Available from: https://www.cdc.gov/diabetes/data/statistics-report/
- 5. Ngo-Metzger Q, Legedza ATR, Phillips RS. Asian Americans’ reports of their health care experiences. Results of a national survey. Journal of General Internal Medicine. 2004;19(2):111–119. https://doi.org/10.1111/j.1525-1497.2004.30143.xArticlePubMedPMC
- 6. American Diabetes Association. Older adults: Standards of medical care in diabetes-2018. Diabetes Care. 2018;41(1):s119–s125. https://doi.org/10.2337/dc18-s011ArticlePubMed
- 7. Weinger K, Beverly EA, Smaldone A. Diabetes self-care and the older adult. Western Journal of Nursing Research. 2015;36(9):1272–1298. https://doi.org/10.1177/0193945914521696Article
- 8. Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: Patient and provider factors. Diabetes Research and Clinical Practice. 2011;93(1):1–9. https://doi.org/10.1016/j.diabres.2011.02.002ArticlePubMed
- 9. Arksey H, O’Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. https://doi.org/10.1080/1364557032000119616Article
- 10. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS medicine. 2009;6(7):e1000097. https://doi.org/10.1371/journal.pmed.1000097ArticlePubMedPMC
- 11. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Loannidis JPA, et al. The PRISMA statement for reporting systematic reviews and meta-analysis of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. https://doi.org/10.1136/bmj.b2700ArticlePubMedPMC
- 12. Chesla CA, Chun KM, Kwan CML. Cultural and family challenges to managing type 2 diabetes in immigrant Chinese Americans. Diabetes Care. 2009;32(10):1812–1816. https://doi.org/10.2337/dc09-0278ArticlePubMedPMC
- 13. Chesla CA, Kwan CML, Chun KM, Stryker L. Gender differences in factors related to diabetes management in Chinese American immigrants. Western Journal of Nursing Research. 2014;36(9):1074–1090. https://doi.org/10.1177/0193945914522718ArticlePubMed
- 14. Chun KM, Chesla CA, Kwan CML. “So We Adapt Step by Step”: Acculturation experiences affecting diabetes management and perceived health for Chinese American immigrants. Social Science & Medicine (1982). 2011;72(2):256–264. https://doi.org/10.1016/j.socscimed.2010.11.010Article
- 15. Chun KM, Kwan CML, Strycker LA, Chesla CA. Acculturation and bicultural efficacy effects on Chinese American immigrants’ diabetes and health management. Journal of Behavioral Medicine. 2016;39(5):896–907. https://doi.org/10.1007/s10865-016-9766-2ArticlePubMedPMC
- 16. Cha E, Yang K, Lee J, Min J, Kim KH, Dunbar SB, et al. Understanding cultural issues in the diabetes self-management behaviors of Korean immigrants. The Diabetes Educator. 2012;38(6):835–844. https://doi.org/10.1177/0145721712460283ArticlePubMedPMC
- 17. Choi SE, Lee JJ, Park JJ, Sarkisian CA. Spousal support in diabetes self-management among Korean immigrant older adults. Research in Gerontological Nursing. 2015;8(2):94–104. https://doi.org/10.3928/19404921-20141120-01ArticlePubMed
- 18. Joo JY, Lee H. Barriers to and facilitators of diabetes self-management with elderly Korean-American immigrants. International Nursing Review. 2016;63(2):277–284. https://doi.org/10.1111/inr.12260ArticlePubMed
- 19. Nam S, Song HJ, Park SY, Song Y. Challenges of diabetes management in immigrant Korean Americans. The Diabetes Educator. 2013;39(2):213–221. https://doi.org/10.1177/0145721713475846ArticlePubMed
- 20. Hu J, Amirehsani K, Wallace DC, Letvak S. Perceptions of barriers in managing diabetes: Perspectives of Hispanic immigrant patients and family members. The Diabetes Educator. 2013;39(4):494–503. https://doi.org/10.1177/0145721713486200ArticlePubMedPMC
- 21. Iten AE, Jacobs EA, Lahiff M, Fernández A. Undocumented immigration status and diabetes care among Mexican immigrants in two immigration “sanctuary” areas. Journal of Immigrant and Minority Health. 2014;16(2):229–238. https://doi.org/10.1007/s10903-012-9741-0ArticlePubMed
- 22. Smith-Miller CA, Berry DC, DeWalt D, Miller CT. Type 2 diabetes self-management among Spanish-speaking Hispanic immigrants. Journal of Immigrant and Minority Health. 2016;18(6):1392–1403. https://doi.org/10.1007/s10903-015-0271-4ArticlePubMed
- 23. Kindarara DM, McEwen MM, Crist JD, Loescher LJ. Health-illness transition experiences with Type 2 diabetes self-management of Sub-Saharan African immigrants in the United States. The Diabetes Educator. 2017;43(5):506–518. https://doi.org/10.1177/0145721717724725ArticlePubMed
- 24. Magny-Normilus C, Mawn B, Dalton J. Self-management of Type 2 diabetes in adult Haitian immigrants: A qualitative study. Journal of Transcultural Nursing : Official Journal of the Transcultural Nursing Society. 2020;31(1):51–58. https://doi.org/10.1177/1043659619841586ArticlePubMed
- 25. McConatha JT, Kumar VK, Raymond E, Akwarandu A. Cultural dimensions of diabetes management: A qualitative study of Middle Eastern immigrants in the U.S. Journal of Cross-Cultural Gerontology. 2020;35(1):85–98. https://doi.org/10.1007/s10823-019-09383-7ArticlePubMed
- 26. Njeru JW, Formea CM, Osman A, Goodson M, Hared A, Capetillo GP, et al. Diabetes knowledge, attitudes and behaviors among Somali and Latino immigrants. Journal of Immigrant and Minority Health. 2016;18(6):1432–1440. https://doi.org/10.1007/s10903-015-0335-5ArticlePubMed
- 27. Park C, Nam S, Whittemore R. Incorporating cultural perspectives into diabetes self-management programs for East Asian immigrants: A mixed-study review. Journal of Immigrant and Minority Health. 2016;18(2):454–467. https://doi.org/10.1007/s10903-015-0181-5ArticlePubMed
- 28. Borhaninejad V, Shati M, Bhalla D, Iranpour A, Fadayevatan R. A population-based survey to determine association of perceived social support and self-efficacy with self-care among elderly with diabetes Mellitus (Kerman city, Iran). The International Journal of Aging and Human Development. 2017;85(4):504–517. https://doi.org/10.1177/0091415016689474ArticlePubMed
- 29. Williams DR. Race and health: Basic questions, emerging directions. Annals of Epidemiology. 1997;7(5):322–333. https://doi.org/10.1016/s1047-2797(97)00051-3ArticlePubMed
- 30. Karter AJ. Race and ethnicity: Vital constructs for diabetes research. Diabetes Care. 2003;26(7):2189–2193. https://doi.org/10.2337/diacare.26.7.2189ArticlePubMed
- 31. Mitchel FM. Racial and ethnic health disparities in an era of health care reform. Health & Social Work. 2015;40(3):e66–e74. https://doi.org/10.1093/hsw/hlv038Article
- 32. Agency for Healthcare Research and Quality. National healthcare disparities report. Research Report. Department of Health and Human Services; 2013 October. Publication No.: 13-0003.
- 33. Digital Repository at the University of Maryland [Internet]. Washington DC: Patient Protection and Affordable Care Act of 2010: Advancing health equity for racially and ethnically diverse populations. [cited 2023 Mar 15]. Available from: https://doi.org/10.13016/t2o2-gn6b
- 34. Lum TYS, Yan ECW, Ho AHY, Shum MHY, Wong GHY, Lau MMY, et al. Measuring filial piety in the 21st century: Development, factor structure, and reliability of the 10‐item contemporary filial piety scale. Journal of Applied Gerontology: The Official Journal of the Southern Gerontological Society. 2016;35(1):1235–1247. https://doi.org/10.1177/0733464815570664ArticlePubMed
- 35. Smedley BD, Stith AY, Nelson AR. Unequal treatment: Confronting racial and ethnic disparities in health care. 1st ed. Washington DC: National Academies Press; 2003. 80 p.
References
Figure & Data
References
Citations


 KACHN
KACHN
 PubReader
PubReader ePub Link
ePub Link Cite
Cite